REVIEW ARTICLE
A scoping review of published reports of the infection prevention and control assessment framework: a comparison to the findings of the global report on infection prevention and control
Peta-Anne Zimmerman1,2,3,4 and Matt Mason3,4,5
1School of Nursing and Midwifery, Griffith University, Gold Coast, Australia; 2Infection Control Department, Gold Coast Health, Gold Coast, Australia; 3School of Health, University of the Sunshine Coast, Sippy Downs, Queensland, Australia; 4Collaborative for the Advancement of Infection Prevention and Control, Queensland, Australia; 5Australian Centre for Pacific Islands Research, University of the Sunshine Coast, Sippy Downs, Queensland, Australia
Abstract
Background: The World Health Organization (WHO) published the Global Report on Infection Prevention and Control (IPC) in 2022, highlighting both achievements and areas for improvement in IPC practices globally. The Infection Prevention and Control Assessment Framework (IPCAF) is a tool used to evaluate IPC programs across different healthcare settings.
Aim: This scoping review aims to identify published reports of IPCAF use, collate available data, and compare findings to those of the WHO’s Global Report on IPC.
Methods: A scoping review methodology was employed, involving searches in PubMed, MEDLINE via Ebsco, CINAHL via Ebsco, Embase via Ovid, and Scopus from November 2016 to March 2024. Studies included were surveys, cross-sectional studies, before-after studies, observational studies, or cohort studies published in peer-reviewed journals. Data extraction focused on study characteristics, IPC Core Component results, and overall IPCAF scores.
Results: Twenty-seven articles met the inclusion criteria, representing 18 countries across four WHO regions. High-income countries (HICs) like Germany, Austria, and Japan reported predominantly Advanced IPCAF scores. In contrast, low-income countries (LICs) such as Sierra Leone, Uganda, and Ethiopia often reported Basic or Inadequate scores. Lower-middle-income countries (LMICs) like India, Indonesia, and Pakistan showed mixed results, while upper-middle-income countries (UMICs) like Türkiye and China generally reported higher scores. The review highlighted significant variability in IPC scores within and between countries.
Conclusion: The findings corroborate the WHO’s Global Report, emphasizing the need for tailored interventions to enhance IPC practices, particularly in resource-limited settings. Addressing gaps in data collection and increasing participation from underrepresented regions are crucial for developing a robust global IPC framework.
Keywords: IPCAF; scoping review; infection prevention and control; core components; IPC programs; low- and middle-income countries
Citation: Int J Infect Control 2025, 21: 23806 – http://dx.doi.org/10.3396/ijic.v21.23806
Copyright: © 2025 Zimmerman and Mason. This is an Open Access article distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for any purpose, even commercially, provided the original work is properly cited and states its license.
Received: 3 October 2024; Accepted: 13 February 2025; Published: 27 March 2025
To access the supplementary file, please visit the article landing page
Competing interests and funding: The authors declare no conflict of interests.
*Peta-Anne Zimmerman, Griffith University, Gold Coast Campus, Parklands Drive, Southport, QLD 4215 Australia. Email: p.zimmerman@griffith.edu.au
In 2022, the World Health Organization (WHO) published the Global Report on Infection Prevention and Control (IPC)(1), which identified both achievements and opportunities for improvement in the provision of patient and healthcare workers’ safety at both country and global levels. At the 75th World Health Assembly, a resolution on IPC was adopted by Member States culminating in the recently published Global Strategy on IPC(2). The foundation for these activities and publications is the WHO Core Components of IPC(3), the Minimum Requirements for IPC Programmes(4), and associated evaluation tools. Of the 194 Member States of the WHO, 106 contributed to the data evaluating the national minimum requirements reported in the Global Report, with only 58 (54.7%) of those countries reporting an active IPC programme, and four (3.8%) meeting all minimum requirements (1). At the healthcare facility level, 4,440 facilities from 81 of the 194 Member States, across all WHO regions, voluntarily participated in the survey using the Infection Prevention and Control Assessment Framework (IPCAF) (1, 5). The IPCAF uses a scoring system out of 800 over the Core Components, where Advanced is 800-601, Intermediate 600-401, Basic 400-201, and Inadequate is 200-0 (5).
The Global Report’s low response rates for both national and facility-based surveys highlighted a pronounced inclination toward the inclusion of high-income countries (HICs) (1). Additionally, it revealed a diverse array of data-gathering techniques, including self-reporting by in-country or healthcare facility staff to desk reviews. A limitation of the Global Report is that participation is limited in some geographical areas, for example, only six out of the 37 Member States in the Western Pacific Region have results reported (1).
Since the publication of the IPCAF in 2018 (5), countries, health services, and facilities have used these tools to assess their own situation to develop action plans for improvement. Some of these assessments have been shared in peer-reviewed publications for the benefit of the wider IPC community. This scoping review aims to identify published reports of IPCAF use, collate available data, and compare findings to those of the Global Report on IPC (1).
Methods
A scoping review was chosen for this study as it examines the state of current research on a topic or phenomenon of interest (6). This is achieved by reviewing available literature, collating, and summarizing the data. Adapted from the six-stage methodology of Arksey and O’Malley (6), five of the six stages were utilized: specify the research question, identify relevant literature, select studies, mapping of the data, and summarize and report the results (6).
Stage 1: Research question
Based upon the aim of this study, the research question was that what reports of use of the IPCAF have been published and how do their findings compare to the Global Report on IPC?
Stage 2: Identification of relevant literature
We conducted searches in the following databases: PubMed, MEDLINE via Ebsco, CINAHL via Ebsco, Embase via Ovid, and Scopus. Dates searched were November 2016 to March 2024. This start date was based upon the date of publication of the WHO Core Components for IPC programmes (3). The search used Boolean operators (see Supplementary material 1). In addition to searching databases, we also manually checked the reference lists of the included studies, performing both forwards and backwards citation analysis. The Systematic Review Accelerator (https://pubmed.ncbi.nlm.nih.gov/32004673/) was used in the design of the search.
Stage 3: Study selection
We included surveys, cross-sectional studies, before-after studies, observational studies (all types), or cohort studies of all published works in peer-reviewed journals. We included studies, published in English, involving reported use of the IPCAF to assess alignment of IPC programmes with the Core Components for IPC Programmes (3). We excluded studies if the IPCAF was adapted to the extent that the data were not comparable to the IPCAF methods. The primary outcome was the results of the IPCAF. We included studies conducted in healthcare facilities or at a national level. Theses and books or book chapters were excluded from the search.
The initial search identified 326 titles, with 85 removed due to duplication (Fig. 1). After the initial title and abstract screen of the remaining 241 by both authors, 205 were excluded. Both authors performed full-text screening on the remaining 36 articles. Eight were excluded as the IPCAF was not used, and one had results that could not be included as the IPCAF data were not able to be defined. A total of 27 articles were included for data extraction. Figure 1 presents the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) for the study selection (7) There were no disputes between authors on article inclusion. Covidence (https://www.covidence.org/) was used to assist with study selection, mapping, and reporting of the data.
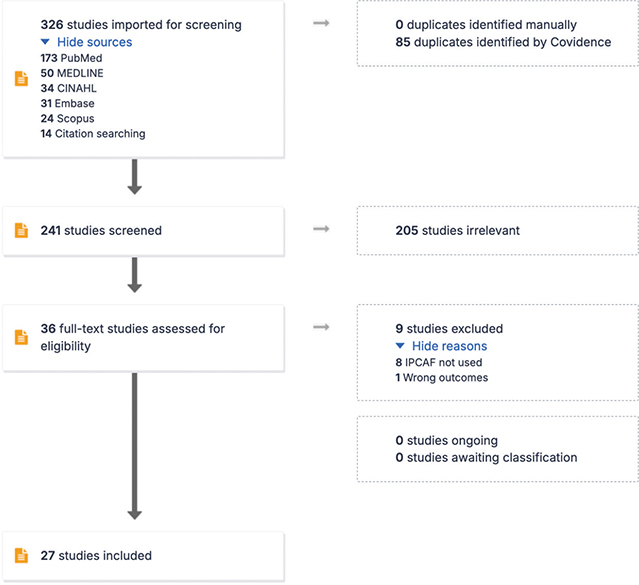
Fig. 1. Article selection based on Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
Stage 4: Mapping of the data
We used a data extraction form for study characteristics and outcome data, which was piloted on two studies in the review. Both authors extracted the following data from included studies: authors, year, country, setting, journal, type of publication, WHO region, World Bank income level, adaptation of the IPCAF, self-report, IPC core component results (where available), and overall IPCAF result (where available). Notes were taken regarding key points of interest or data explanations (Supplementary material 2). Quality of the articles was not assessed as we used the same tool for all articles for assessment. We did not contact investigators or study sponsors to provide missing data.
Results
Stage 5: Summary and report of the findings
Twenty-seven articles met the inclusion criteria for the final scoping review. All articles used the IPCAF, with two of the 27 adapted (0.07%). Ten out of the 27 were published in 2023, nine in 2022, four in 2021, and two each in 2020 and 2019. The majority were from the African region (n = 12), including Uganda, Cote d’Ivorie, Ethiopia, Nigeria, Sierra Leone, and Ghana, followed by South-East Asia (n = 7), including India, Indonesia, Bangladesh, and Pakistan; Europe (n = 5), including Austria, Germany, Türkiye, Italy, and Armenia; and the Western Pacific (n = 3), including Japan, Papua New Guinea, and China. Eleven of the 27 included studies were from low-income countries (LICs), eight from lower-middle-income countries (LMICs), and four each from upper-middle-income countries (UMICs) and HICs. Five were conference abstracts from peer-reviewed conferences. The journal publishing most reports to date is ‘Antimicrobial Resistance and Infection Control’ (n = 8) with studies from the Western Pacific (Papua New Guinea, Japan, and China), South-East Asia (Indonesia and Bangladesh), and Europe (Austria, Germany, and Türkiye).
There were nine reports of overall Advanced scores (n = 4 HI: Europe n = 2, Western Pacific n = 2; n = 2 UMI: Europe n = 1, South-East Asia n = 1; n = 2 LMI South-East Asia; n = 1 LI African), nine Intermediate (n = 1 HI Europe; n = 1 UMI, n = 2 LMI: African region n = 1, South-East Asia n = 1; n = 5 LI African region), six Basic scores (n = 3 LMI: Western Pacific n = 1, South-East Asia n = 2; n = 3 LI African region), and three reported overall Inadequate scores (n = 1 LMI South-East Asia; n = 2 LI African region). The number of published IPCAF audits reports by World Bank Income Level and WHO region are collated in Fig. 2.
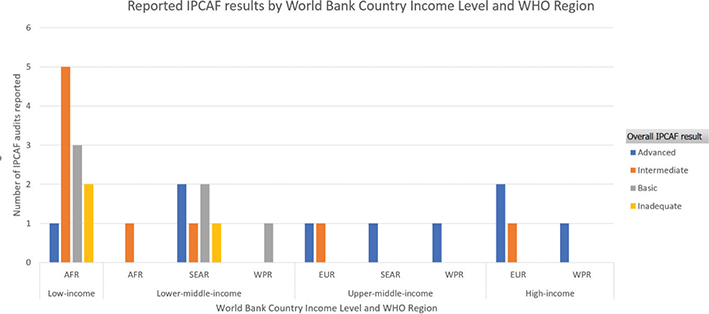
Fig. 2. IPCAF results by World Bank country income level and the World Health Organization region.
LMICs like India, Indonesia, and Pakistan presented a mixed picture. In India, Katoch et al. (8) reported a median overall score of 620.0, with a range of Basic to Advanced scores across different facilities. Supriadi et al. (9) in Indonesia found a median overall score of 620.0, with the majority of facilities scoring Advanced or Intermediate. Pakistan, as reported by Tahir et al., (10) showed a median overall score of 405, with scores ranging from Inadequate to Advanced, reflecting variability in IPC practices across different facilities.
UMIC such as Türkiye and China generally reported higher scores. For instance, Azak et al. (11) in Türkiye found median scores ranging from 70.0 to 98.8 across core components, with an overall Advanced score. In China, Ni et al. (12) reported median scores of 655 for secondary hospitals and 720 for tertiary hospitals, both in the Advanced range.
The range of geographical regions and income levels reflects a diverse set of contexts in which the IPCAF has been applied. For instance, HICs like Germany, Austria, and Japan reported predominantly Advanced IPCAF scores, indicating strong IPC programmes. In Germany, the study by Aghdassi et al. (13) reported Advanced scores across all core components, with mean scores ranging from 71.3 to 96.1. Similarly, in Austria, Aghdassi et al. (14) found Advanced scores with mean scores between 57.6 and 95.7. Japan also reported Advanced scores, with Nomoto et al. (15) showing median scores ranging from 60.0 to 100 across different core components.
In contrast, studies from LICs such as Sierra Leone, Uganda, and Ethiopia often reported Basic or Inadequate scores, highlighting significant challenges in IPC implementation. For example, the study by Margao et al. (16) in Sierra Leone showed improvements over time, with mean scores increasing from 27.0 to 83.0 in different core components between 2021 and 2023, yet still reflecting a need for substantial improvement. Similarly, Opollo et al. (17) in Uganda reported Basic scores across most core components, with scores as low as 0.0 in several areas.
A common theme across the studies is the variability in IPC scores within and between countries, influenced by factors such as income level, healthcare infrastructure, and the specific challenges faced by each region. HICs generally reported stronger IPC programs, while LMICs showed more variability and often lower scores, indicating areas needing significant improvement.
Discussion
The findings of the scoping review underscore the importance of tailored interventions and support to enhance IPC practices, particularly in resource-limited settings.
This scoping review identified 27 published reports from 18 different countries on use of the IPCAF to assess IPC programme alignment with the WHO IPC Core Components. These reports represented four of the six WHO regions, with no published reports from the Eastern Mediterranean or the Americas. Most published reports indicated an overall IPCAF assessment score of either Advanced or Intermediate (66.6%, n = 18). All identified HIC reports (13–15, 18) were included in this with 75% having an Advanced level, which is reflective of the Global Report findings (1). Interestingly, nearly half of LMIC and LIC reports in the literature sit within the Basic (10, 17, 19–22) (n = 6) and Inadequate (23–25) levels (n = 3) unlike the findings of the Global Report which indicate most LMIC sit primarily in the Intermediate range with LIC primarily in Basic (1). This discrepancy could be due to differences in data collection methods, or the specific studies included in the review.
This discrepancy could also be attributed to the availability and accuracy of data to contribute to a global report (1). The results for the Western Pacific Region in the Global Report are a case in point where there is a significant lack of data available from the majority of the member states. Missing data from the Eastern Mediterranean and the Americas beg an explanation for their absence. Hence, the Global report must be considered in this context, being incomplete and not fully representative of either global or regional situations, a limitation the report itself recognizes (1). For specific IPC knowledge and context, there remains a reliance on published works, which, to date, is also not well represented in the literature. What is published demonstrates a clear bias to HICs, where resources are available to support such IPC and publishing activities (26).
The Global Report emphasized the significant burden of HAIs in LMICs, where the incidence is higher compared to HICs. This is consistent with the findings of the scoping review, which identified a higher prevalence of Basic and Inadequate scores in LMICs. Both the scoping review and the Global Report noted low participation rates, especially from LICs, which could bias the findings toward HICs. The Global Report used a mix of self-reporting and desk reviews, similar to the methods identified in the scoping review. Additionally, both sources highlighted a lack of data from certain regions, such as the Eastern Mediterranean and the Americas, underscoring the need for more comprehensive data collection efforts in these areas.
The positive impact of effective IPC programs on reducing HAIs and improving patient safety was emphasized in both the scoping review and the Global Report. The Global Report provided more detailed data on the cost-effectiveness of IPC programs, which could be a valuable addition to the discussion. Overall, the findings of this scoping review corroborate the Global Report’s conclusions while highlighting specific areas where further research and targeted interventions are needed to improve IPC practices globally. By addressing the gaps and challenges identified in both the scoping review and the Global Report, a more robust and effective global IPC framework can be achieved.
Recommendations
Based on the findings from the scoping review and the comparison with the WHO’s Global Report on IPC, several recommendations can be made to enhance IPC practices globally. First, efforts should be made to increase participation and data collection from underrepresented regions, such as the Eastern Mediterranean and the Americas. This could involve targeted outreach and support to these regions to encourage participation in IPC assessments. Standardizing data collection methods across countries and facilities is crucial to reduce bias and improve the reliability of data. This could involve providing clear guidelines and training for self-reporting and desk reviews.
Second, based on the results and looking forward, it would be reasonable to suggest targeted interventions should be developed to address the specific challenges faced by LMICs, particularly those with Basic and Inadequate IPCAF scores. This could include providing resources, training, and support to improve IPC practices. Highlighting and learning from the success stories of LMICs that have achieved Advanced or Intermediate scores can help other countries improve their IPC programs. Investing in the training and education of healthcare workers on IPC practices is essential, involving comprehensive training programs and continuous professional development opportunities. Encouraging the development of local IPC experts who can lead and sustain IPC initiatives within their own countries and regions is also important.
Third, more studies and reports on IPC assessments should be encouraged, especially from underrepresented regions and LMICs, to build a more comprehensive global understanding of IPC practices. Creating platforms for knowledge exchange and collaboration among countries and regions, such as international conferences, workshops, and online forums, can facilitate the sharing of experiences and solutions. Countries should align their national IPC policies with WHO guidelines and recommendations, including adopting the WHO Core Components of IPC and the Minimum Requirements for IPC Programs. Regular monitoring and evaluation of IPC programs are essential to ensure their effectiveness and identify areas for improvement, involving periodic assessments using tools like the IPCAF.
This scoping review has several limitations that should be acknowledged. First, the inclusion of only English-language studies may have resulted in the exclusion of relevant research published in other languages, potentially introducing language bias. Second, the reliance on self-reported data in many of the included studies may have introduced reporting bias, as facilities might overestimate their compliance with IPC standards. Additionally, the variability in data collection methods across studies, including differences in the adaptation of the IPCAF tool, may have affected the comparability of results. The review also highlighted a pronounced inclination toward HIC, which could bias the findings and limit the generalizability to low- and middle-income countries. Furthermore, the lack of published reports from certain regions, such as the Eastern Mediterranean and the Americas, underscores the need for more comprehensive data collection efforts in these areas. Finally, the quality of the included studies was not assessed, which may affect the reliability of the findings. Future research should aim to address these limitations by including a broader range of languages, standardizing data collection methods, and ensuring more representative participation from diverse geographical regions and income levels.
Conclusion
The WHO’s Global Report on IPC (1) provided a comprehensive analysis of IPC programs worldwide, emphasizing the effectiveness of good IPC practices in reducing HAIs by up to 70%. The report highlighted the significant burden of HAIs, particularly in LMIC, where the incidence is higher compared to HIC. It also discussed the impact of AMR and the cost-effectiveness of IPC programs. Both this scoping review and the Global Report noted low participation rates, especially from LIC, which could bias the findings toward HIC. The Global Report used a mix of self-reporting and desk reviews, similar to the methods described in the review. With both sources highlighting a lack of data from certain regions, it underscores the need for more comprehensive data collection efforts in these areas. Both the scoping review and the Global Report emphasized the positive impact of effective IPC programs on reducing HAIs and improving patient safety. The Global Report provided more detailed data on the cost-effectiveness of IPC programs, which could be a valuable addition to the discussion.
References
| 1. | World Health Organization. Global report on infection prevention and control. Geneva: World Health Organization; 2022. |
| 2. | World Health Organization. Global strategy on infection prevention and control. Geneva: World Health Organization; 2023. |
| 3. | World Health Organization. Guidelines on core components of infection prevention and control programmes at the national and acute health care facility level. Geneva: World Health Organization; 2016. |
| 4. | World Health Organization. Minimum requirements for infection prevention and control programmes. Geneva: World Health Organization; 2019. |
| 5. | World Health Organization. Infection prevention and control assessment framework at the facility level. Geneva: World Health Organization; 2018. |
| 6. | Arksey H, O’Malley L. Scoping studies: towards. methodological framework. Int J Soc Res Methodol 2005; 8(1): 19–32. doi: 10.1080/1364557032000119616 |
| 7. | Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021; 372: n71. doi: 10.1136/bmj.n71 |
| 8. | Katoch O, Katyal S, Srivastav S, Rodrigues C, Rupali P, Chakrabarti A, et al. Self-reported survey on infection prevention and control structures in healthcare facilities part of a national level healthcare associated infection surveillance network in India, 2019. Am J Infect Control 2022; 50(4): 390–5. doi: 10.1016/j.ajic.2021.09.019 |
| 9. | Supriadi IR, Haanappel CP, Saptawati L, Widodo NH, Sitohang G, Usman Y, et al. Infection prevention and control in Indonesian hospitals: identification of strengths, gaps, and challenges. Antimicrob Resist Infect Control 2023; 12(1): 6. doi: 10.1186/s13756-023-01211-5 |
| 10. | Tahir MA, Khan MA, Ikram A, Chaudhry TH, Jabeen A, Quddous A, et al. Assessment of infection prevention and control (IPC) implementation and strategies used for IPC preparedness at facility level in underdeveloped areas of Pakistan. Infect Drug Resist 2023; 16: 1997–2006. doi: 10.2147/idr.S399830 |
| 11. | Azak E, Sertcelik A, Ersoz G, Celebi G, Eser F, Batirel A, et al. Evaluation of the implementation of WHO infection prevention and control core components in Turkish health care facilities: results from a WHO infection prevention and control assessment framework (IPCAF)-based survey. Antimicrob Resist Infect Control 2023; 12(1): 11. doi: 10.1186/s13756-023-01208-0 |
| 12. | Ni K, Jin D, Wu Z, Sun L, Lu Q. The status of infection prevention and control structures in Eastern China based on the IPCAF tool of the World Health Organization. Antimicrob Resist Infect Control 2022; 11(1): 46. doi: 10.1186/s13756-022-01087-x |
| 13. | Aghdassi SJS, Hansen S, Bischoff P, Behnke M, Gastmeier P. A national survey on the implementation of key infection prevention and control structures in German hospitals: results from 736 hospitals conducting the WHO Infection Prevention and Control Assessment Framework (IPCAF). Antimicrob Resist Infect Control 2019; 8: 73. doi: 10.1186/s13756-019-0532-4 |
| 14. | Aghdassi SJS, Grisold A, Wechsler-Fördös A, Hansen S, Bischoff P, Behnke M, et al. Evaluating infection prevention and control programs in Austrian acute care hospitals using the WHO Infection Prevention and Control Assessment Framework. Antimicrob Resist Infect Control 2020; 9(1): 92. doi: 10.1186/s13756-020-00761-2 |
| 15. | Nomoto H, Saito H, Ishikane M, Gu Y, Ohmagari N, Pittet D, et al. First nationwide survey of infection prevention and control among healthcare facilities in Japan: impact of the national regulatory system. Antimicrob Resist Infect Control 2022; 11(1): 135. doi: 10.1186/s13756-022-01175-y |
| 16. | Margao S, Fofanah BD, Thekkur P, Kallon C, Ngauja RE, Kamara IF, et al. Improvement in infection prevention and control performance following operational research in Sierra Leone: a before (2021) and after (2023) study. Trop Med Infect Dis 2023; 8(7): 376. doi: 10.3390/tropicalmed8070376 |
| 17. | Opollo MS, Otim TC, Kizito W, Thekkur P, Kumar AMV, Kitutu FE, et al. Infection prevention and control at Lira University Hospital, Uganda: more needs to be done. Trop Med Infect Dis 2021; 6(2): 69. doi: 10.3390/tropicalmed6020069 |
| 18. | Montella E, Iodice S, Bernardo C, Frangiosa A, Pascarella G, Santalucia I, et al. Integrated system for the proactive analysis on infection risk at a university health care establishment servicing a large area in the south of Italy. J Patient Saf 2023; 19(5): 313–22. doi: 10.1097/pts.0000000000001141 |
| 19. | Harun MGD, Anwar MMU, Sumon SA, Hassan MZ, Haque T, Mah-E-Muneer S, et al. Infection prevention and control in tertiary care hospitals of Bangladesh: results from WHO infection prevention and control assessment framework (IPCAF). Antimicrob Resist Infect Control 2022; 11(1): 125. doi: 10.1186/s13756-022-01161-4 |
| 20. | Kamara IF, Tengbe SM, Fofanah BD, Bunn JE, Njuguna CK, Kallon C, et al. Infection prevention and control in three tertiary healthcare facilities in Freetown, Sierra Leone during the COVID-19 pandemic: more needs to be done! Int J Environ Res Public Health 2022; 19(9): 5275. doi: 10.3390/ijerph19095275 |
| 21. | Tognon F, Manenti F, Putoto G, Scanagatta C. Application of infection prevention and control assessment framework (IPCAF) tool in 13 hospitals in sub Saharan Africa. Trop Med Int Health 2021; 26(SUPPL 1): 120. |
| 22. | Marme G, Kuzma J, Zimmerman P, Harris N, Rutherford S. Tuberculosis infection prevention and control in rural Papua New Guinea: an evaluation using the infection prevention and control assessment framework. Antimicrob Resist Infect Control 2023; 12(1): 31. doi: 10.1186/s13756-023-01237-9 |
| 23. | Ashuro Z, Washo G, Diriba K. Indoor air quality in hospital settings. London: IntechOpen; 2023. |
| 24. | Cissé DM, Laure EEM, Blaise KA, Paul NNJ, Gbonon MV, Mayaka CRA, et al. Evaluation of the implementation of hospital hygiene components in 30 health-care facilities in the autonomous district of Abidjan (Cote d’Ivoire) with the WHO Infection Prevention and Control Assessment Framework (IPCAF). BMC Health Serv Res 2023; 23(1): 870. doi: 10.1186/s12913-023-09853-2 |
| 25. | Savul S, Lalani FK, Ikram A, Khan MA, Khan MA, Ansari J, et al. Infection prevention and control situation in public hospitals of Islamabad. J Infect Dev Ctries 2020; 14(9): 1040–6. doi: 10.3855/jidc.12779 |
| 26. | Woods WA, Watson M, Ranaweera S, et al. Under-representation of low and middle income countries (LMIC) in the research literature: Ethical issues arising from a survey of five leading medical journals: have the trends changed? Glob Public Health 2023; 18(1): 2229890. doi: 10.1080/17441692.2023.2229890 |