REVIEW ARTICLE
Do reusables pose greater infectious risks than disposables for consumer goods? A systematic literature review
Sanjidah Ahmed Ira1, Brooke Sherry2, Ruhana Amin3, Ma-sum Abdul-Hamid4, Timothy Roberts5, Sarah Hochman6 and Cassandra L. Thiel7*
1Tandon School of Engineering, New York University, Hicksville, NY, USA; 2Department of Population Health, NYU Langone Health, New York, NY, USA; 3NYU Tandon School of Engineering, Ozone Park, NY, USA; 4New York University, Saadiyat Island, Abu Dhabi, United Arab Emirates; 5Health Sciences Library, NYU Langone Health, New York, NY, USA; 6Department of Medicine, NYU Grossman School of Medicine, New York, NY, USA; 7Department of Population Health, NYU Langone Health, New York, NY, USA
Highlights
- Very few studies specifically assess the safety or infectious risks of reusable and single-use food serviceware.
- In general, pathogens will survive on most fomites, especially those with higher porosity and in higher humidity settings.
- The literature does not point to reusable containers as major pathogen transmission sources; thus bans on reusable items may be inappropriate.
- As the adoption of reusable serviceware increases, protocols and guidelines for the general public should be established to help maintain health and safety.
Abstract
Increased concern over climate change and the emergence of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) virus resulted in a clash of political directives around reusable and disposable food serviceware. Decreasing single-use items will likely reduce consumption and environmental emissions; however, improper cleaning of reusable items could result in greater risks of disease transmission. We sought to assess the risks of reusable and disposable food serviceware and document disinfection protocols by conducting a systematic literature review of articles that assessed materials or products that could be fomites to specific food-borne pathogens. After initial screening, the study team extracted data from 122 articles. The most common pathogens studied were E. coli (25% of included studies), general bacteria (24%), and Norovirus (16%). Thirteen studies (8%) focused on SARS-CoV-2. A majority of studies analyzed plastics (27%), stainless steel (22%), or porous surfaces such as paper and cardboard (12%). Forty seven of the studies (35%) were conducted in a food service setting, and 40 studies (30%) tested disinfection techniques. Despite a large body of related literature, there is very little evidence suggesting that either reusable or disposable food serviceware is safer for minimizing infectious risks. Pathogens can survive on various fomites, though greater surface porosity and higher humidity levels increase viability of most pathogens. There appear to be no major differences in pathogen viability on various fomites. There is a paucity of research that can specifically aid in developing policy or guidelines for appropriate use of reusable food serviceware. Though given recent studies on SARS-CoV-2, banning reusable bags and food serviceware is an inappropriate response to this particular pathogen, which is rarely spread through surface contact. Further research is needed that explicitly studies pathogen viability, transmission risks, and appropriate disinfection techniques for disposable and reusable food serviceware in order to devise effective sustainability policies.
Keywords: single-use plastic; reusable; food service; pathogens; fomites; infection; sustainability
Citation: Int J Infect Control 2024, 20: 23758 – http://dx.doi.org/10.3396/ijic.v20.23758
Copyright: © 2024 Sanjidah Ahmed Ira et al. This is an Open Access article distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for any purpose, even commercially, provided the original work is properly cited and states its license.
Received: 3 September 2023; Revised: 8 October 2023; Accepted: 8 October 2023; Published: 7 October 2024
Competing interests and funding: This research was funded by Break Free From Plastic. Authors report no other potential conflicts.
*Cassandra Thiel, Assistant Professor, NYU Langone Health, 227 E 30th St. #636, New York, NY 10016. Email: Cassandra.thiel@nyulangone.org
In recent years, there has been increasing concern over the growth of single-use and disposable consumer plastics consumption and the resulting environmental and health issues.1,2 First developed in the 1800s, plastic production has exploded from 2 million metric tons in 1950 to 348 million metric tons in 2017, and is expected to double in production rate by 2040.3 Driven by convenience, cost, and perceived safety, consumer products and their packaging are often made of single-use and disposable plastics. Of the 335 million metric tons of global plastics produced in 2016, 5% was used to make carrier bags, 6% for plastic bottles, 4% for household goods, and 2% for food services disposables.3 Most plastics are manufactured from fossil fuel-based feedstocks, leading to a variety of environmental pollution as a result of oil and gas extraction.4 Though generally considered stable, plastics are known to leach hormone-mimicking chemicals called phthalates which can disrupt biological systems and cause cancers in humans and other animals.5 Plastic end-of-life has much to be desired, with one study estimating that of the ~6.3 billion metric tons of plastics ever made only about 9% has been recycled.2 Geyer et al. estimate 12% has been incinerated, releasing hazardous air pollutants such as dioxins,6 and 79% has accumulated in landfills or the natural environment.2 Single-use plastics are some of the most commonly found litter during beach clean ups and are estimated to make up 60–95% of global marine plastic pollution.7 With a flourish of media attention, The Ellen MacArthur Foundation released a report estimating that by 2050, there will be more plastic in the ocean than fish, by weight.1
In response to these alarming statistics, many retail stores began to encourage customers to bring reusable bags or reusable containers for coffee and leftover food. In addition, many federal, state, and local governments targeted single-use plastics in the food service sector, creating regulations that disincentivized or banned items such as plastic grocery bags, plastic straws, and polystyrene takeout containers.
Many of these policies were quickly reversed in early 2020, however, as the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) (coronavirus disease 2019 [COVID-19]) pandemic emerged. Many grocery stores prohibited reusable shopping bags and restaurants and coffee shops banned reusable takeout containers, for fear of spreading the virus causing COVID-19.
The Plastics Industry Association submitted a letter to the US Department of Health and Human Services, citing three studies that highlighted the potential of reusable bags to carry and transmit pathogens; however, none of the studies referenced investigated coronaviruses, such as SARS-CoV-2.8 One study looked at a single outbreak of norovirus, a very contagious gastrointestinal (GI) virus, but was unable to differentiate between the handling of the food and the handling of the bag containing the food.9 The other two studies explore potential for contamination inside reusable bags, and not transmission risks to staff and other customers using the bags. Both recommend regular washing of bags and other hygienic protocols be encouraged with the general public.
The harms of single-use plastics on public health and the natural environments on which humans depend should be addressed, and they need to be balanced with the potential risks of spreading pathogens in the consumer goods and food service sector. Therefore, this study systematically reviews existing scientific literature focused on the viability of SARS-CoV-2, as well as common pathogens causing foodborne illness, on common food-contact surfaces (fomites). Study fomites include carryout bags, reusable and single-use foodware, and the different materials used in these products. We examine the literature to determine transmission risk and effective decontamination strategies for specific pathogens, as well as to identify opportunities for further research to inform safe and environmentally sustainable alternatives to single use consumer plastics in the food sector. It is our hope that by better understanding the risks of various pathogens on multiple types of surfaces in the food service sector, we might design a system that is both safe AND environmentally sustainable.
Methods
Following the PRISMA guidelines for systematic reviews, in October 2021, a trained medical librarian (TR) performed searches for studies without language or date restrictions in the Medline, Inspec, and Embase databases. (Medline search strategy available in Appendix.) The citations of relevant Systematic Reviews and included studies were screened for additional studies. Abstract and full text screenings were completed in Covidence systematic review software by at least two members of the research team (HB, MS, ML, YG), using the inclusion and exclusion criteria shown in Table 1. Conflicts were resolved through consensus. Data were extracted from each included paper by two members of the research team (MS, MT, RA, YG) with any discrepancies addressed by a third reviewer. Studies were excluded if they focused exclusively on hospital acquired infections such as Staphylococcus aureus or Pseudomonas aeruginosa, and water-borne pathogens (as from wastewater treatment). After an initial screening process, the team decided to expand exclusion criteria to remove papers focused on antimicrobial properties of silver and copper, studies that may have fomites (specifically plastics) mentioned above but focused on a medical setting, and studies where the fomite was solely hands or cell phones. Additionally, non-English studies were excluded during full text review.
Results
Demographics of included studies
After duplicates were removed, the initial search yielded 1,138 results for title/abstract screening (Fig. 1). A total of 435 studies were excluded at the full text screening stage, leaving 122 articles that met all inclusion criteria.
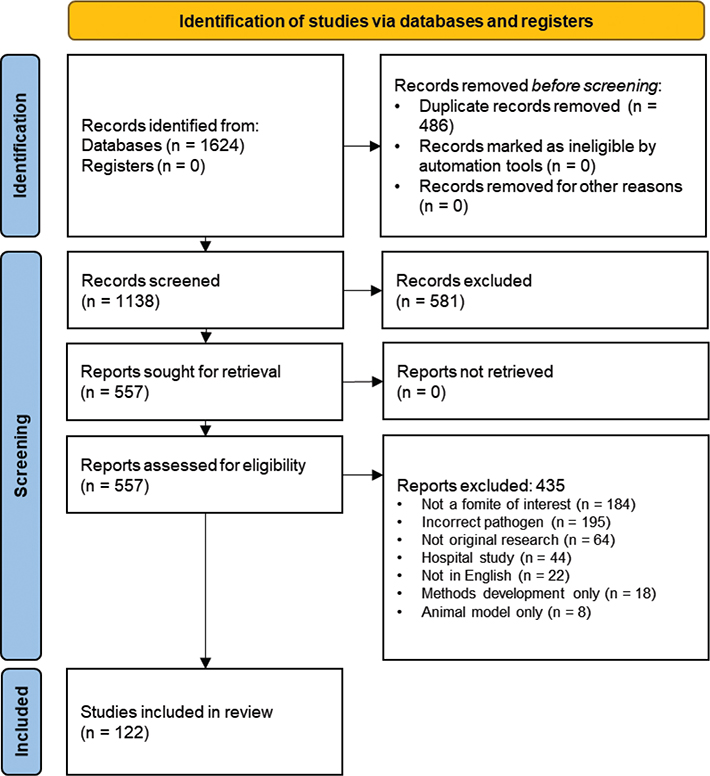
Fig. 1. PRISMA flow diagram for systematic review of pathogens on food service related fomites.10
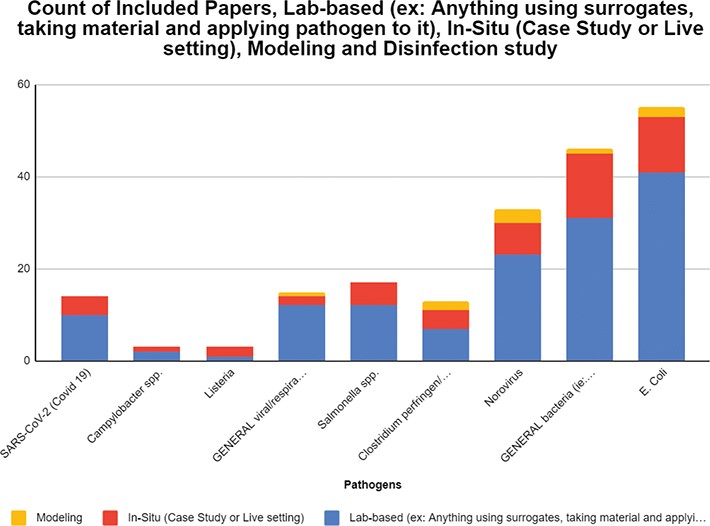
Forty seven studies (35%) were conducted in a food service setting, 30 (22%) in a hospital setting, 20 (14%) in a general commercial or household setting, and 34 (25%) in unspecified settings or contexts (several studies considered multiple settings). The most common pathogens found in the complete dataset were E. coli (25% of included studies), general bacteria (24%), and Norovirus (16%). Thirteen studies (8%) focused on SARS-CoV-2.
A majority of studies analyzed plastics (76 studies, 27%), stainless steel (61, 22%), or porous surfaces such as paper and cardboard (33, 12%). A majority of plastics studied were unspecified (21, 30% of this subset), polypropylene (14, 20%), non-specified polyethylene (12, 17%), or polystyrene (8, 12%). Most common ‘natural’ materials included cloth such as cotton or hemp (22, 41% of this subset) and wood (18, 33%).
Most studies were lab-based (101, 75% of total), followed by in-situ tests (30, 22%), and models (5, 4%). Most studies assessed the presence of pathogens (96, 72%), while 12 (9%) assessed transmissibility, and 16 (12%) assessed both presence and transmissibility. Forty studies (30%) tested disinfection techniques (see Appendix for related figures and tables).
Though we had no date exclusion criteria, the earliest study included was published in 1978. It appears that these studies are increasing over time, with a plurality, perhaps unsurprisingly, in 2020 (Fig. 2). These studies were published in 60 unique journals, with seven articles each in The Journal of Hospital Infection, PloS One, and the International Journal of Food Microbiology.
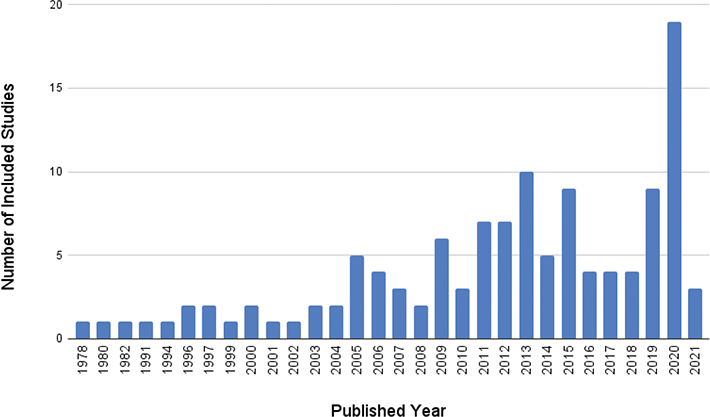
Fig. 2. Number of included studies by year of publication.
A majority of the studies reported support from federal grants (53, 38%), with 20 (14%) reporting industry sponsors and 40 (29%) not listing any funding support. Most studies were conducted in the United States or by researchers from the US (49, 40%), the United Kingdom (13, 11%), or Canada (7, 6%). The remaining 53 studies (43%) were conducted in 29 unique countries.
Pathogen viability and transmissibility from various fomites
Given the variation in viability and transmissibility by pathogen, the following section summarizes study results by pathogen. Any studies conducted on more than one pathogen will be summarized in the appropriate sections. A summary of transmissibility studies is shown in Table 1.
Escherichia coli
Escherichia coli (E. coli) are Gram negative bacteria commonly found in the environment and in the lower gastrointestinal tract. They represent a large and diverse group of bacteria. While most strains are harmless in the gastrointestinal tract, some strains can cause diarrheal illness or more severe systemic disease. Of the papers selected for inclusion, E. coli was studied in 48 (40%) of the included papers. A total of 41 papers were conducted in a lab setting and seven papers were in-situ. A total of 15 of the 48 papers analyzed a disinfection method. The fomites discussed in these studies include plastics (34), natural/porous material (21), metal (19), stainless steel (15), glass (9), and porcelain/ceramic (8). Of the 48 papers that were selected as E. coli studies, only five of them involved food-related fomites.
Fomite features that can influence microbial adhesion include surface energy and topography. All surfaces have a charge that can create interactions with other surfaces. Usually, the smaller the structures, the more the interactions that can form between the fomite and the structure (such as bacteria).11 One study investigated adhesive characters of bacteria, swab features, and fomite surface properties in terms of contamination and bacterial colony counts. The fomites studied in this experiment were untreated planed wood, plastic computer tower, acrylic painted wall, glass, aluminum, wrestling mat squares, and ethylene-vinyl acetate footwear.11 The greatest retrieval of bacteria was from the acrylic surface and the least retrieval was from the wood. This is because a rough surface/topography decreases adhesion of the bacteria to the surface compared to a smooth surface/topography.11 Therefore, retrieval was highest for the acrylic fomite.
Attachment to the surface can also vary based on the bacterial species itself. One study investigated the transfer efficiency of Acinetobacter baumannii from contaminated nitrile gloves to polypropylene plastic. It was found that A. baumannii could transfer from the gloves 3 min after inoculation of bacteria to the plastic, even after the glove surface was dried completely.12 A. baumannii is able to attach and form biofilm structures on plastic and glass surfaces but E. coli is not able to form these attachments as easily. The glove material also influenced transfer efficiency as when conducting an experiment using latex gloves instead of nitrile, transfer efficiency was higher for latex (1.6% vs. 0.2%).12 Oxygen treatment on surfaces can create a hydrophilic surface that reduces bacterial adhesion by 68.7% as found in another study. This oxygen treatment along with fluorine reactive ion etching treatment on the surface allowed for a 99.6% reduction of E. coli cell adhesion compared to the control polypropylene plastic surface.13
One study investigated the transfer efficiency of bacteria from porous and nonporous surfaces under different relative humidity conditions. The porous surfaces tested were cotton, polyester, and paper currency (one dollar bills), and the nonporous surfaces tested were acrylic, glass, ceramic tile, laminate, stainless steel, and granite.14 It was found that transfer efficiencies were greater under high relative humidity conditions compared to low relative humidity conditions. It was also found that fomite type did influence transfer as porous surfaces are able to better trap organisms, and provide a much greater surface area for adherence. Specifically, transfer efficiency was up to 57% for porous surfaces and less than 6.8% for nonporous surfaces under low humidity conditions and up to 79.5% for porous surfaces and less than 13.4% for nonporous surfaces under high humidity conditions.14
Some surfaces may have antimicrobial activity and can be effective against certain bacteria. In one study, copper was found to demonstrate antimicrobial activity against all bacteria studied in the experiment, including E. coli, Enterobacter spp., Klebsiella pneumoniae, Pseudomonas aeruginosa, and Acinetobacter baumannii.15 E. coli was found to be inactivated within only a few minutes of being exposed to the copper surfaces. It was found that a higher copper content of alloys (Cu99% vs. Cu63%) and a dry inoculation technique as opposed to wet, increased contact killing, decreasing viability and subsequent transfer.15 Another study similarly found that copper has strong antimicrobial properties. However, it has poor corrosion resistance and is unsuitable as a surface material. Nickel or silver that contain copper do have improved durability and can greatly reduce bacterial survival. In one study, after 120 min of exposure at 20 degrees Celsius and 360 min at 4 degrees Celsius, E. coli could not be detected on a copper nickel surface.16
Campylobacter Spp.
Campylobacter are Gram negative bacteria that are the most common bacterial cause of diarrheal illness in the United States. Campylobacter can be acquired from eating undercooked meat, unpasteurized milk, or by eating contaminated fruits or vegetables. Of the papers selected for inclusion, three (2%) studied Campylobacter. Two of these papers were conducted in a lab setting and one in-situ. Two of the three papers analyzed a disinfection method. The fomites discussed in these studies include plastics like polypropylene (1), natural/porous material like paper or cardboard (1), cloth (1), metal (1), glass (1) and porcelain/ceramic (1).
Campylobacter was found to be most prevalent on plastic and wood, according to a study investigating the killing of Campylobacter on contaminated wooden cutting boards by glycerol monocaprate.17 Past research shows that wood has an antibacterial effect. This may be due to moisture being naturally drawn into the board and therefore bacteria tend to be less viable on wood compared to other materials. The glycerol monocaprate sanitizer tested in this study had difficulty entering the pores of the wood, which allowed more bacteria to survive.17 Because plastic is a nonporous surface, the bacteria were more viable on this material, as liquid cannot pass through the plastic as is possible with wood.
Another study investigated the cross-infection of potential food pathogens in the domestic kitchen during chicken preparation.18 The study tested 325 sampling sites after 25 chickens were prepared, 11 of which were contaminated with Campylobacter. For the homes where there was Campylobacter contamination, the maximum contamination was found on draining boards (four homes), followed by counter tops and hands (three homes), and oven handles (two homes).18 In another study, it was hypothesized that Salmonella and Campylobacter may be able to survive a typical washing-up process and persist on dish surfaces. The factors affecting the survival of Campylobacter and several other bacterial strains during a washing-up process were investigated. It was found that Campylobacter survived least well compared to E. coli, which survived the best.19 The Campylobacter cells were most sensitive to towel drying and did not recover on these dried dishes after a washing-up process.19 However, some sterile dishes washed subsequent to contaminated dishes did contain Campylobacter, indicating that transfer of bacteria through washing-up water can occur.19
Clostridium perfringens and Clostridioides difficile
Clostridium perfringens bacteria are a common cause of food poisoning. C. difficile bacteria can cause a diarrheal illness, especially in healthcare settings or in people who have recently taken antibiotics. Both of these bacteria form spores that allow them to survive in the environment, and both can produce toxins in the gastrointestinal tract and cause diarrhea. Ten of the included papers (8%) studied C. difficile or C. perfringens. Of these, seven were lab-based, and four were in-situ. Eight papers assessed disinfection techniques. The fomites discussed in these papers included stainless steel (6), plastic (4), fabric (2), and glass (1). It was found that C. difficile was viable on all of these surfaces.
In one disinfection study where the efficacy of a pulsed xenon disinfection device was being investigated, it was found that at baseline, the glass slides were contaminated with 5 log10 CFU of bacteria.20 One study measured the effect of Perasafe (a high-level disinfectant that generates peracetic acid in-situ when dissolved in water) and sodium dichloroisocyanurate (NaDCC) against spores of C. difficile on stainless steel and polyvinyl chloride.21 It was found that Perasafe was significantly more active than NaDCC against C. difficile spores dried on stainless steel surfaces and was less effective against C. difficile spores fixed on polyvinyl chloride floor covering material. This may suggest that C. difficile spores are more viable on the polyvinyl chloride surface compared to stainless steel.21 Another study investigated the prevalence of Clostridium difficile on retail surfaces and shoppers’ plastic bags. A total of 800 samples were taken from 17 supermarkets in Saudi Arabia. It was found that C. difficile’ prevalence on sampled surfaces was overall 0.75% and that the highest prevalence was found on retail baskets and trolleys, followed by plastic bags last.22 Though only 3 isolates/400 were obtained from plastic bags, it was concluded that C. difficile is present in surfaces in retail supermarkets and can contaminate shoppers’ plastic bags.22
Listeria
Listeria are Gram positive bacteria that are widespread in the environment. Unlike most other foodborne pathogens, Listeria can grow at standard refrigerator temperatures, which makes it more of an infection risk in refrigerated ready-to-eat foods. Listeria can cause febrile gastroenteritis in people with normal immune systems, but it can cause invasive infection in older and immune compromised people, and in pregnant women can cause miscarriage or sepsis in the neonate. Three of the included papers (2%) focused on Listeria. Of these, one paper was lab-based and two were in-situ. None of the papers mentioned disinfection methods. The fomites discussed in these studies include plastic (2), fabric (2), natural/porous material (1), metal (1), silicone (1), cutting boards (1), and kitchen utensils (1).
Listeria was most prevalent on wet surfaces, like dish clothes and places of stagnant water. One study investigated the prevalence of Salmonella, Staphylococcus aureus, Bacillus cereus, Clostridium perfringens, Listeria monocytogenes, and fecal coliforms like E. coli in 15 food and hand contact surfaces in 250 randomly chosen domestic kitchens in Wageningen, Netherlands.23 Listeria monocytogenes was found in 10% of the houses investigated and were mainly isolated from wet surfaces like dish cloths and places of stagnant water.23 Likewise, another study found Listeria on cleaning tools, mainly those that could retain moisture. This study evaluated the association of multiple types of bacteria with cleaning tools (floor mops), cleaning cloths, and handling devices (disposable plastic gloves) used to fill baguette and assorted salad preparation in four retail delicatessens in Johannesburg, South Africa.24 Floor mops consistently yielded the highest APCs (aerobic plate count), CCs (coliform counts), ECs (Escherichia coli counts), while gloves had the lowest corresponding counts. Listeria was detected in five cleaning tool samples.24 Bacterial attachment occurs more readily to surfaces in moist environments. Because the floor mops and cleaning cloths remained moist, the environment for bacterial attachment and growth on the mops and cleaning cloth fibers was provided.24
Salmonella Spp.
Salmonella are Gram negative bacteria with several subspecies that cause human disease. Salmonella often live in the intestinal tracts of animals and can be transmitted to humans through consumption of food contaminated with animal feces. Very old, very young, and immunocompromised individuals are at higher risk for complications from Salmonella infection. Of the papers selected for inclusion, a total of eight studies (7%) studied Salmonella. Of these eight papers, five were conducted in a lab-setting, and three studies were conducted in-situ. Five of the eight papers were food service setting papers. Two studies analyzed various disinfection techniques. The fomites discussed in these studies include porous material like paper, fabric or cloth (5), plastic (4), glass (3), metal (2), stainless steel (2), porcelain/ceramic (2), and wood (1).
According to the CDC, many foodborne outbreaks occur in restaurants and can be due to contaminated food and poor personal hygiene. In a study exploring the persistence of Salmonella on the surface of restaurant menus, Salmonella was found to survive on laminated menus for up to 72 h and not paper menu coupons.25 In follow-up studies exploring the transmissibility of Salmonella from contaminated menus to fingertips and from the fingertips to clean menus, it was found that microorganisms could be transferred from damp menus to fingertips for up to 24 h.25 There is also a higher transfer of bacteria from wet surfaces. This was also found in another study that studied mops and cloths as potential reservoirs for bacterial contamination. It was found that bacterial attachment to surfaces occurs more readily in moist environments, and the floor mops and cleaning cloths used in the study were kept moist.24 Salmonella was detected on three of the cleaning cloths and two mop samples, and these cleaning tools may transfer microorganisms to food contact surfaces and contaminate food in restaurants.24
Studying the resistance of various bacterial species in dry conditions is important as well. Salmonella can survive air-drying for at least 24 h.19 In one study, it was found overall that Gram-negative bacteria lose their viability in the air faster than Gram-positive bacteria.10 When adding protein such as bovine serum albumin, however, bacterial survival increased even when the bacteria was dried.10 This effect was seen in Salmonella. One study exploring cross-contamination of food-borne pathogens in Salmonella-infected chicken preparation, found 100% contamination on places in the kitchen such as the counter-top and dishcloth.18 When comparing various fomites, one study found that stainless steel may be the best surface to prevent bacterial contamination on cutting boards in comparison to plastic and wooden cutting boards.26 This could be because the harder metallic surface of stainless steel makes it difficult for bacteria to attach.
In conclusion, there are many factors that can cause foodborne infection, such as: preparation of food too far in advance, improper cooling, and inadequate heating.23 However, cross-contamination via various fomites is highly likely, and, as such, it is important that proper hygiene is always followed to reduce risk of transmission.
General bacterial pathogens (Gram negative or positive)
A total of 42 (34%) of the included papers focused on general bacterial pathogens. Of these, 31 were lab-based, 14 were in-situ, and 1 was a modeling study. A total of 14 papers were disinfection studies, of which 10 were lab-based, seven were in-situ, and one was modeled. The fomites that were discussed in a plurality of studies include: plastic (31), fabric (16), metal (12), stainless steel (11), cloth (11), wood (8), glass (7), and aluminum (3).
Bacterial viability is not only due to the fomite it is present on, but also due to the bacterium strain, temperature, and humidity. In all 43 papers, different strains of general bacteria were present and able to survive on the fomites investigated in the studies. The presence and viability of different pathogens on dry surfaces was investigated in multiple papers and it was found that bacteria can survive on dry surfaces regardless of the material. In one study, the survival of Acinetobacter baumannii on dry surfaces was investigated. The survival curve of the bacteria was found to be significantly associated with the specific strain of bacteria rather than material.27 Ten strains of bacteria were studied on ceramic, polyvinyl chloride, rubber, and stainless steel in dry conditions. It was found that the recoverable proportion of the strains on the different materials did differ greatly, with 12% on ceramic to 96% on rubber, with an average of 46% of inoculated microorganisms recovered.27 When looking at the influence of materials on the recoverable portion and reduction by drying, no influence was found in association with survival curves.27 There was a significant association between survival curve and bacterial strain, instead.
In another study, the effect of thermal control of dry fomites on regulating the survival of human pathogenic bacteria was investigated and it was found that the colony forming units of the bacteria decreased only if the temperature increased.28 Vinyl chloride, stainless steel, and aluminum were the fomites in this study, and there was no difference in bacterial counts between these three materials. Bacteria tended to favor a lower temperature regardless of the fomite, even in dry conditions. However, temperature may not always affect the viability of bacteria, as it was found in one study that Yersinia enterocolitica populations did not change across varying temperatures and soil conditions. The serum in the soil had a protective effect on L. monocytogenes but did not cause the same growth and survival for all bacteria. In this study, it was shown that survival was more dependent on pathogen type.29 In another study, cleaning tools were studied as it was hypothesized that they may play a role in the contamination of foods without proper hygiene, and it was found that the most bacteria were found on floor mops compared to disposable plastic gloves.24 It was thought that this was the case because bacteria need moisture to grow and the floor mops and cleaning cloths had been diluted in a sanitizer when they were not being used for cleaning.24
As for specific fomites, studies found bacteria were viable on plastic, stainless steel, glass, and wood, though the most bacterial contamination was often found on plastic fomites. Bacteria can survive for several weeks on plastic after drying.30 In one disinfection study focused on the safety of hardwood cutting boards in food preparation it was found that between maple, beech, and plastic cutting boards, the plastic boards were the most contaminated with bacteria with a mean count of 41 CFU/cm2 compared to 7.5 CFU/cm2 for maple and 23.5 CFU/cm2 for beech.31 In a similar study of cutting boards, bacteria survived best on plastic and glass and were not viable on wood.32 When looking at wood, it was found that oak exhibited an antibacterial effect and that after cultivation, bacteria could not be found on the wood after 48 h. When studying stainless steel that was composed of 74% iron, 18% chromium, and 8% nickel, it was found that at room temperature and refrigeration temperature, bacteria survived for more than 28 days in a desiccated state. The inhibitory effects of 21 copper-containing alloys was also tested on cultures of E. coli and it was found that copper can have an antibacterial effect due to its corrosive nature. As copper content, or temperature or relative humidity increased, it was found that the bacteria survived less.16
Norovirus
Norovirus is a highly infectious virus that causes acute gastroenteritis with vomiting and diarrhea after ingestion. It is spread by eating contaminated food, by touching contaminated surfaces and then touching the mouth, and can be spread from person to person. Thirty one (25%) of the papers studied Norovirus. Of these 31 papers, 20 were lab-based, five were in-situ, one paper was modeling, two papers were a combination of lab-based and modeling, one paper was a combination of lab-based and in-situ, and two papers were a combination of in-situ and modeling. Furthermore, 11 of the papers were disinfection studies. The fomites discussed in these studies include: stainless steel (30), plastic or plastic resin (17), porcelain/ceramic (8), fabric (7), natural or porous material (5), glass (5), metal (3), nitrile/rubber (3), latex (2), and vinyl (2).
The studies mostly point towards the same conclusion: that norovirus is viable on most fomites for long periods of time. One study found that norovirus consistently survived longer on wood, when observing the inactivation rates of norovirus over varying temperature and humidity levels on rubber tree wood and stainless steel.33 Specifically, it was found that norovirus consistently survived longer on wood compared to stainless steel at a lower temperature. One study found that the presence of food residues on fomites may elongate viability of norovirus on fomites. This study evaluated the survivability of norovirus (murine norovirus-1) on desiccated food residue-attached stainless steel coupons.34 Food residue included lettuce, cabbage, and ground pork. The study found that a 6.2 log MPS/ml of MNV-1 was completely lost at day 30 in residue-free coupons, whereas only a 1.4 log MPN/ml reduction was observed in coupons with residues.34
Several studies point to the fact that norovirus outbreaks may be more of a result of improper cleaning protocols and improper hygiene practices. One study found that the initial cleaning of dorm rooms tied to a norovirus outbreak, by cleaning staff uninformed on proper cleaning protocols for norovirus, actually increased the amount of norovirus-positive rooms from 40 to 73%.35 In another study, often cited by those advocating for single-use consumer plastics,8 a norovirus outbreak was found to be associated with coming into contact with a contaminated reusable grocery bag. This study investigated a reported norovirus outbreak that affected nine members of a soccer team. The outbreak was associated with contact with a reusable grocery bag and/or consuming its packaged food contents. The bag and its contents were previously stored in a bathroom used by a person with norovirus-like symptoms.
Even though it was found that contaminated surfaces do play a role in transmission and as virus donors, this is to a lesser extent compared to contaminated hands themselves as vehicles of virus transmission. One simulation model evaluated the contribution of fomite-mediated exposures to infection and illness risks in outbreaks, accounting for hand-to-porous surfaces, hand-to-nonporous surfaces, hand-to-mouth, -eyes, -nose, and hand washing events.36 Infection risks ranged from 70.22 to 72.20% and illness risks ranged from 21.29 to 70.36%, with the number of hand-to-mouth contacts and the number of hand washing events having the strongest relationships with model-predicted doses. This model suggested that fomites accounted for 25–82% of illnesses in an outbreak.36 Overall, this study concluded that fomite-mediated exposures accounted for a large portion of the attack rates in outbreaks that involve various transmission modes,36 but proper gloving and hand-washing compliance are the most effective in controlling contamination of food products from norovirus.37 Norovirus can be readily transferred from the hands to other surfaces such as food, being the most efficient route.37
SARS-CoV-2
SARS-CoV-2 is a respiratory virus that causes COVID-19, with symptoms ranging from mild upper respiratory tract infections to acute respiratory disease syndrome and death. SARS-CoV-2 can be transmitted through respiratory droplets and aerosols, and to a lesser extent through fomites. Of the 13 SARS-CoV-2 related papers, 11 measured prevalence of virus on fomites, one measured transmissibility, and one measured both. Nine studies were conducted in a lab setting, three in-situ, and one both lab and in-situ. The most prevalent fomites include plastic (9 studies, either unspecified (3) or PP (3)), stainless steel (5), glass (4), and cloth or fabric (3).
All four in-situ studies found the presence of SARS-CoV-2 RNA (ribonucleic acid) on a wide range of fomites,38–40 including wooden chopsticks. One study concluded that prevalence of SARS-CoV-2 RNA on various fomites correlated with the patient’s viral load, whether the patient was symptomatic or asymptomatic.41 Of the four in-situ studies, only one measured viability, finding that none of the collected samples had infectious titers of SARS-CoV-2 when added to tissue culture assays.40
The 10 lab-based studies assessed adhesion, decay rate, and disinfection techniques for SARS-CoV-2 on various fomites. One study found that SARS-CoV-2-inoculated plastic surfaces retained the ability to infect cells for up to 84 h at both room temperature and 28 C.42 Two studies found that increasing temperatures and humidity drastically reduced the survivability of the virus to as little as 24 h at 40ºC.43,44 Droplet volume and surface type (stainless steel, plastic, nitrile glove) were not found to significantly impact decay rate.44 However, one study found that SARS-CoV-2 took up to 20 days more to degrade on experimentally-inoculated plastic personal protective equipment (PPE) when compared to 100% cotton fabric.45 Similarly, according to a study focused on intermolecular interactions between SARS-CoV-2 and surfaces using atomic force microscopy under simulated respiratory droplet environment, polystyrene (plastics) showed strongest adhesion, followed by stainless steel, gold, and glass.46
General viral pathogens
Fourteen (11%) of the included studies assessed general viral/respiratory pathogens. Of these, 12 were lab-based and two were in-situ; three papers were disinfection studies. The fomites that were discussed in a majority of these studies include plastic or plastic resin including polypropylene, polyvinyl chloride, polyester and polystyrene (9), metal (8), stainless steel (8), fabric (3), porcelain/ceramic (3), glass (2), silicone (1), cloth (1), and aluminum (1).
One study tested the effect of both high and low humidity on the transfer of pathogens from a fomite (surface) to finger from various common surface types. Nine fomites were investigated in this study and they comprised six nonporous and three porous surfaces. It was found that, overall, viral pathogens had higher transfer efficiencies in high relative humidity for all surface types, compared to low relative humidity.14 It was also found that a nonporous surface (acrylic, glass, ceramic tile, laminate, stainless steel, and granite) had a much higher transfer efficiency under high and low relative humidity for all types of surfaces. The transfer efficiency under high relative humidity for a nonporous surface was up to 57% compared to less than 0.6% for a porous surface. Under low relative humidity, the transfer efficiency for a nonporous surface was up to 79.5% compared to less than 13.4% for a porous surface.14 Four different organisms were studied in this paper including E. coli, Polioivirus (serotypes 1 and 2), B. thuringiensis, and Emesvirus zinderi or Bacteriophage (MS2) coliphage. Fomite type affects transfer efficiency rates for all of these organisms except PV-2. It is suggested that the reason porous surfaces have much lower transfer efficiency rates is because they can trap organisms and have a higher surface area. This was found to be the case in another study where bacteriophage Phi 6 was being studied, and it was shown to survive longer on nonporous surfaces compared to porous surfaces.47 Another study studied the inactivation rates of murine norovirus (MNV), MS2 and hepatitis A virus (HAV) on wood and stainless steel under various temperatures and humidity conditions. It was found that the viruses survived longer on wood at low temperatures and were not as viable on stainless steel. This was thought to be the case because stainless steel is hydrophilic and carries a negative surface charge, creating stress for microbe survival.33 Though the survival of the viruses depended on more factors than just surface type, such as virus type and temperature, overall the results of the study indicated that the viruses were able to survive for more than 1 month.33
Another study investigated the survival of HAV on six fomites including ceramic, rubber, glass, wood, stainless steel and plastic.48 Survival was measured up to 28 days, and it was found that the virus survived the longest on the wood, followed by rubber, plastic, ceramic, glass and for the least amount of time on stainless steel. On the other hand, another study showed that several influenza viruses survived the longest on stainless steel. In this study, three surfaces were studied which were stainless steel, microfiber cloth, and cotton. The virus strains survived on the steel for 174.9 h, 34.3 h on the microfiber cloth, and 17.7 h on the cotton.49 In terms of transmissibility, it was found that quantities of influenza A could be transferred from stainless steel to an individual’s hands for a period of 1 day after the steel is contaminated. However, the virus can only survive on the hands for up to 5 min, so this was concluded to be a limited amount of time for pathogen transmission into the mucous membranes to cause respiratory illness.49,50 Another study investigated the virucidal action of disinfectants assayed against hepatitis A and human rotavirus which were dried onto polystyrene. Polystyrene was used as a fomite so that the behavior of enteric viruses on nonporous surfaces could be studied, and it was shown that these viruses were viable on the polystyrene.51 Another study also investigated hepatitis A and human rotavirus as well as adenovirus and poliovirus, and virus survival on various surfaces. The surfaces included paper, cotton, aluminum, china, glazed tile, latex and polystyrene. It was concluded in this study that the four viruses were able to survive on all of the surfaces for prolonged periods of time. It was found that HAV and human rhinoviruses (HRV) were more resistant to inactivation than Adenovirus (ADV) and PV when dried onto the various surfaces. Specifically with HAV, inactivation rates were found to be higher on porous surfaces compared to nonporous surfaces.52 In one study, RSV was specifically looked at and it was found that RSV could be recovered from countertops and gloves for the longest periods (average of 7 and 5 h respectively). Survival rate diminished greatly as on cloth, the virus was recovered for an average of 2 h and on the skin and paper tissue, survival was diminished to an average of 30 min.53
Fomite disinfection techniques
Thirty nine studies assessed the effectiveness of disinfection techniques on various pathogens and fomites.
Energetic treatment
Five studies assessed the effectiveness of disinfection techniques that use ultraviolet radiation and photocatalytic inactivation to disinfect a variety of fomites or surfaces. Energetic treatments are not chemical processes, but rather effective physical processes to render microorganisms such as bacteria, viruses, yeasts, and fungi harmless within seconds.
Photocatalytic inactivation
One study found that modified titanium films were found to be most efficient in bacteria inactivation at the starting concentration of 105–106 CFU/ml. Photoinactivation was not observed under visible light irradiation of titanium oxide coatings. After 8 h of irradiation in the presence of catalytic titanium oxide, the concentration of E. coli decreased by a factor of 103. It was demonstrated that catechol-photosensitized titanium oxide films can be used as potential antimicrobial coatings.54
Ultraviolet radiation
Pulsed xenon ultraviolet disinfection was found to be effective in reducing the recovery of MRSA and C. difficile within a 10-min exposure time.31 As the distance increased between the device and the pathogens, the device did not work as efficiently. Compared to ultraviolet C radiation, UV-C achieved significantly greater log10CFU reductions than the PX-UV device. Ultraviolet radiation applied for 120 s using the UVSC equipment was effective in disinfecting slides inoculated with four microorganisms involved in healthcare-associated infections such as P. aeruginosa, E. coli, S. aureus, and C. albicans. The effect was even greater against spore-forming B. subtilis, obtaining an effect similar to that of 70% ethanol and 2% chlorhexidine.
However, UV-C devices do contain mercury which can be toxic to people in the hospital; therefore the pulsed xenon ultraviolet device has advantages. Furthermore, UV-C cannot be used when people are present in the room. This is interesting to note because UV-A can be used at moderate doses with people present in the room, and can still cause reductions in bacterial count.55 At an irradiance of 3 W/m2 there was a progressive reduction in recovery of the vegetative microorganisms over 24 h in comparison to untreated controls. After 8 h of exposure to UV-A, MRSA and MS-2 were reduced by >1 log10 CFU or PFU, whereas Candida auris was reduced by 0.7 log10 CFU. Phi X174 was reduced by only 0.6 log10 PFU over 24 h.
It was also found in a study that the effectiveness of UV light is very dependent on the specific surface/fomite that is being disinfected. When using the disinfection technique on Formica laminate and stainless steel, it was found that inactivation on Formica laminate was much lower than on steel. It was also found that inactivation of bacteria and viruses on hard surfaces differed from inactivating microorganisms in liquids. To properly disinfect microorganisms regardless of the fomite, UV light doses would have to be adjusted.56
Dishwasher/heat
Heat is a very common and effective way to sanitize and disinfect objects and various fomites from various pathogens, particularly in residential settings. Heat is effective as when the temperature is high enough, this causes the enzymes in microorganisms to denature which leaves them unable to infect other organisms. One study assessed the effect of heat on pathogens. The creation of heat through a boiling technique was found to be the most effective in inactivating microorganisms and able to cut back the overall counts by 9.9–4.7 log CFU/sponge (50%), whereas the usage of hypochlorite (a chemical treatment) reduced the overall bacterial counts by 8.8–6.8 log CFU/sponge (31%). Heat was found to be more effective than a medical care blanching agent. One study measured the safety of using several disinfection techniques on cutting boards. The three types of cutting boards tested included maple wood, beech wood, and polyethylene hard plastic. The plastic boards were cleaned using an industrial dishwasher and standard detergent, and the wood boards were hand washed with tap water, washing liquid, and a soft cloth. Before cleaning, it was found that the maple and beech boards had the least bacteria, with a mean count of 7.5 and 23.5 CFU/cm^2 of aerobic mesophilic microorganisms. The plastic board has the most bacteria with a mean count of 41 CFU/cm^2 of aerobic mesophilic microorganisms. After cleaning, 23 out of 30 of the samples had less than 2.5 CFU/cm^2 of aerobic mesophilic microorganisms. The study concluded that proper cleaning and disinfection of utensils was necessary to minimize cross-contamination effects. The wooden boards were found to entrap bacteria in the cracks of the board, as a result of constantly cleaning the wooden boards in the dishwasher under harsh conditions. Because plastic harbored more bacteria than the wooden boards, it is recommended to follow the cleaning instructions specific to the materials or products in use (i.e. hand cleaning wood products instead of using a dishwasher).31
Chemical treatment
Chemical disinfectants are used to inactivate pathogens on inert surfaces. The most common chemical disinfectants include alcohol, hypochlorite, and hydrogen peroxide. Ethanol and isopropanol are the main alcohols used as disinfecting agents to target a wide range of bacteria, viruses, and fungi. Hydrogen peroxide is a peroxide-based disinfectant that denatures proteins by oxidizing disulfide bonds and denaturing them. These various chemical disinfectants are widely available and used in the household as they have low toxicity, are inexpensive, and are able to inactivate a wide range of pathogens. A total of 47 studies assessed chemical treatment techniques.
Hydrogen peroxide
Hydrogen peroxide is a commercially available, stable and effective disinfectant that has been used to clean various surfaces for decades. One study used 30% hydrogen peroxide vapor and found that after exposure to vapor, all materials tested including vinyl flooring, ceramic tile, and plastic showed a 4 log 10 reduction in viral titre within 20 min.57 When cleaning glass, plastic or ceramic tile surfaces, an exposure time of 15 min was required.57 Hydrogen peroxide vapor, however, was found to be least effective against feline calicivirus (FCV) on stainless steel.57
Overall, it was found that hydrogen peroxide vapor was suitable for disinfection of various surfaces contaminated with norovirus and influenza viruses including H1N1.58 One study tested hydrogen peroxide vapor and found that even at a low vapor concentration of 10 ppm, a 2-log10 reduction was observed after only 2.5 min of exposure.58 After 2.5 min, exposure to 10-ppm HP vapor resulted in 99% inactivation.58 For air saturated with triethylene glycol (TEG) vapor, the disinfection rate was about 16 times faster.58
Sodium bicarbonate, sodium chlorite, sodium hypochlorite
Sodium hypochlorite, sodium bicarbonate, and sodium chlorite are very common chemical disinfectants. Sodium hypochlorite was found to be very effective across multiple studies and was shown to reduce microbial population significantly compared to no disinfectant on various types of fomites, including plastic, stainless steel, and others. Sodium hypochlorite was found to be effective in reducing FCV and MNV by using 5 ml of the disinfectant for a contact time of 5 min. Through the use of sodium hypochlorite (5,000 ppm), FCV and MNV were both inactivated below the limit of detection on fabric, cloth, plastic, and glass.59 Sodium chlorite was also found to be effective in virus disinfection which induced a 3 log titre reduction of HAV and HRV in most scenarios.51 However, chlorine dioxide was found to be more effective than sodium chlorite. When studying the lethality of sodium chlorite and chlorine dioxide against E. coli O157:H7 on stainless steel, glass, plastic and wooden surfaces, chlorine dioxide was able to kill E. coli with greater efficacy with the exception of wooden surfaces. In one study, sodium bicarbonate was mixed with other disinfectants and the efficacy of these techniques was tested. The various disinfectants tested included sodium bicarbonate + glutaraldehyde, sodium bicarbonate + activated dialdehyde, and sodium bicarbonate + hydrogen peroxide at various concentrations. It was found that increasing the concentration rendered the sodium bicarbonate to be more effective. Thus, 5% sodium bicarbonate was a rapid virucidal agent killing greater than 99.22% FCV in 1 min while a 2% concentration took 10 min to kill 99.60% of FCV. Sodium bicarbonate alone at 5% concentration or a combination of sodium bicarbonate with glutaraldehyde or activated dialdehyde inactivated 99.99% of the virus load from food contact surfaces in a short contact time.
Alcohol. Compared to dry cleaning with cellulose tissues and microfabric clothes the efficacy of alcoholic lenses was much higher when compared to the alcohol-free formulation. It was found that wet cleaning was much more effective than mechanical cleaning with dry wipes.60 One study specifically studied the contamination and disinfection of soft surfaces in health care settings.60 Soft surface sanitizer that contained ethanol was successful in lowering the heterotrophic plate count (HPC) bacterial burden on soft surfaces and also in urgent care facilities and physician’s offices. It was found that the soft surface sanitizer showed an overall 99.99% reduction of seeded microbes in laboratory-controlled studies. A 95–98% reduction of HPC bacteria was achieved with the most effective disinfection on waiting room chairs.60 Another study tested the efficacy of various disinfecting agents on healthcare workers’ pagers.61 One of the disinfecting agents used was 70% vol/vol isopropyl alcohol wipes. The 0.5% chlorhexidine–70% isopropyl alcohol wipes were found to be effective in eliminating all bacterial growth. The next most effective was isopropyl alcohol. Ammonium compounds were also effective but not as effective as the isopropyl alcohol. It was found that after disinfection, no pathogens were found on any of the pagers.61
Other disinfection techniques
Non-ionized or ionized X without or with β-pinene
The results of this study indicate the relative antimicrobial effects of diffuse ionized gaseous species and volatile bactericidal compounds in the vapor phase. The combination of an ionizing source, such as a corona discharge or a candle flame, with a bactericidal volatile has a greater effect on surface-borne bacteria than either treatment alone.62
Oxidative chlorine
Average available chlorine contents of the halogen-activated SS-HACM-Cl coupons, used for antimicrobial efficacy analysis, were measured as 9.6 × 1,016 ± 1.9 × 1,016 atoms/cm2.63 The SS-HACM-Cl stainless steel coupons provided a complete inactivation of about 6 logs (the limit of detection for the antimicrobial assay) against S. aureus and E. coli O157:H7 bacteria within 15 min of contact time in all three replicate assays. These results showed superior inactivation time and efficacy against both Gram-positive and Gram-negative bacteria when compared to previous antimicrobial modified stainless steel surfaces.
Ozone
Ozone disinfection is an extremely strong method for eliminating harmful pathogens. An ozone generator can be used to create reactive ozone from oxygen already in the atmosphere. That reactive ozone can be used to damage bacteria and viruses, which can stop them from causing infections. The findings of one study demonstrate that ozone at 25 ppm and RH 90% is bactericidal to strains of bacteria that commonly cause nosocomial infection, and the bactericidal effect was accomplished with a short exposure (20 min).64 The ozone generator can provide a valuable decontamination tool for the removal of bacteria in many communal settings, including hospitals and other health care institutions.
Soap
Soap is the most common and convenient method in the home to eliminate germs on the hands and washable surfaces. Soap is composed of molecules with hydrophilic heads and tails and is effective at destroying the surface membranes of some bacteria and viruses, including the coronavirus. When washing the hands, microorganisms surround the surface of the hand and the hydrophobic tails wedge themselves into certain microbes and viruses. This destabilizes the bacteria and viruses.
In one study, soap and chlorhexidine (CHG) were equally effective at preventing initial contamination of the basins compared with tap water.65 The qac-positive MRSA strain was recovered in slightly higher numbers in CHG-A and CHG-B compared with the other bacterial species (median, 0.5 CFUs/cm2 for MRSA vs. 0 CFUs/cm2 for other bacterial species; P = 0.057).65 The negative control basins (tap water without bacterial inoculum) yielded extremely low values in both the immediate effect and the residual effect tests, and data are not reported.65 CHGA and CHG-B had a marked residual effect on bacterial contamination compared with soap or tap water (P < 0.0001).65 There was no significant difference in residual activity between CHG-A and CHG-B. When results from basins containing CHG-A and CHG-B were combined, there was no difference in median bacterial counts for the four tested species of bacteria (P = 0.23).65
Another study tested the effectiveness of killing Campylobacter on contaminated plastic and wooden cutting boards using glycerol monocaprate/monocaprin and washing-up liquids (WUL).66 WULs are thick soapy liquids. It was found that viable Campylobacter counts were reduced below the detectable level on plastic board surfaces after treatment with monocaprin (MC) emulsions with or without WULs. It was also found that mixtures of MC-WUL were highly bactericidal on surfaces contaminated with E. coli and that these mixtures were stable at low temperatures. In future studies, mixtures of MC and body soaps or bathroom cleaners should be studied to further determine their microbicidal activities.66
TEG saturated air
TEG vapor can be used to kill odor-causing bacteria for the purpose of air sanitation. It has been found that under optimal conditions, which is about 15–40% relative humidity and 40–100% of glycol vapor, TEG vapor can cause rapid bactericidal action.58 It can possibly be used in conjunction with surface contamination simultaneously even when a room is occupied with people. Vapor concentrations of 10 ppm HP or 2 ppm TEG can provide effective surface disinfection. At these low concentrations, the potential for damage to even the avionics of an airplane would be expected to be minimal. At a TEG vapor concentration of 2 ppm, there are essentially no health risks to people. Vapor concentrations of 10 ppm HP or 2 ppm TEG can provide effective surface disinfection.
Discussion
Though we set out to determine the microbial and infectious risks of food serviceware including reusable shopping bags, cups, and food containers, the literature leads us to no strong conclusions. There appear to be no major differences in pathogen viability on various fomites. There is a paucity of research that can specifically aid in developing policy or guidelines for appropriate use of reusable food serviceware. Though given the recent studies on SARS-CoV-2, banning reusable bags and food serviceware is an inappropriate response to this particular pathogen, which is typically spread through droplets and aerosols, and rarely through surface contact.8 The only other obvious takeaway from existing literature is that any material – reusable or disposable – present in the room of someone infected with norovirus should be properly cleaned and sanitized before use to avoid transmission.
Of the disinfection techniques studied, the most likely to be available for everyday use in the home would be soap and sodium bicarbonate (baking soda). Soap, likely combined with hot water, is sufficient at reducing pathogen load on a majority of studied fomites, suggesting that commercial dishwashing that meets health codes should be sufficiently safe for public health. The literature seems to identify ultraviolet light as the most efficient sterilization technique, and, outside of drying items in the sun, this is not a readily available approach for households, especially for disinfecting reusable food serviceware. A majority of disinfection techniques in the included literature are not accessible to or feasible for the general public. Most of this literature focused on the efficacy of certain disinfection methods common in the hospital space. Surprisingly, none of the included literature assessed the impact of laundering on cloth products, though perhaps our inclusion and exclusion criteria omitted these types of studies.
Sustainability and single-use plastics
Plastics have great utility, but most are currently overused and undervalued, especially within the food service and retail industries. Though sometimes considered a by-product of the oil industry, the plastics industry drives approximately 6% of annual global oil production. In 2019, the production and incineration of new plastics results in over 850 million metric tons of GHGs.1,4 In addition, plastics pose significant environmental risks as macro and micro pollutants and as sources of endocrine disrupting chemicals, risks that are not currently accounted for in life cycle assessments and other environmental impact methodologies.2
Circularity or ‘circular economy’ is a popular framework, promoted by the Ellen MacArthur Foundation and others, which would see the recovery and reuse of plastic resources (and other resources) through reuse, recycling, and proper composting of bio-based plastics, among other tactics.4 Unfortunately, plastics recycling is currently an unreliable market that can exacerbate social inequities, globally, while further polluting ecosystems. Bio-based plastics and their potential composting can also be problematic, as most products must be industrially composted, which may not be a treatment pathway available to most consumers. Single use plastic bans should not be considered an ‘end-all’ for sustainability in the food service sector, but they have been found to catalyze waste awareness and environmental action amongst the general public. Policies banning single-use plastics can be an important tool to curb environmental pollution, especially when combined with proper information and infrastructure for maintaining safety with reusable replacements.
Limitations of our study
The scope of this study made for a challenging systematic review. By including multiple fomites and many pathogen types, we found that measurement techniques and other study methods varied substantially. Though we have tried to summarize major findings, future systematic reviews may focus on a single fomite or a single pathogen for better comparisons between studies. Due to the breadth of potential studies, we may have missed some studies in our selected search terms. In addition, some of the inclusion criteria ended up being somewhat subjective, as we hoped to capture both common reusable and disposable food service products AND the materials that make those products. This led to a challenge in whether or not we should include studies focused on hospital gowns, for example. These gowns are typically composed of a polypropylene fabric, which is a material that could also be used in reusable shopping bags. However, the hospital setting is a very different use case when compared to an individual’s home, a grocery store, or a restaurant. For this reason, we decided to exclude studies that focused on hospital-acquired infections, as these were unlikely to be encountered in our use case setting. The study team also did our best to collect literature on SARS-CoV-2, but as the literature is quickly evolving, there may be more recent studies which we were unable to include.
Conclusion
Despite a large body of related literature, there is very little evidence suggesting that either reusable or disposable food serviceware is safer for minimizing infectious risks. Very few studies focused specifically on the question of safety of reusable versus disposable food serviceware. Various pathogens can survive on various fomites, though greater porosity of the surface and higher humidity levels seem to increase viability of most pathogens. Proper cleaning protocols – including hand hygiene – appear to be the major factor in minimizing infectious risks from any pathogen.
As society at large struggles to reduce the environmental impact of human systems, we must identify safe opportunities to reduce plastic pollution. Eliminating single-use plastics and replacing them with reusable substitutes is a viable opportunity; however, existing literature does not help inform the cleaning and disinfection protocols that should be recommended for everyday people. Further research is needed which explicitly studies pathogen viability, transmission risks, and appropriate disinfection techniques for disposable and reusable food serviceware in the consumer goods space in order to devise effective sustainability policies.
References
| 1. | Neufeld L, Stassen F, Sheppard R, Gilman T. The new plastics economy: rethinking the future of plastics. World Economic Forum; 2016. |
| 2. | Geyer R, Jambeck JR, Law KL. Production, use, and fate of all plastics ever made. Sci Adv 2017; 3(7): e1700782. doi: 10.1126/sciadv.1700782 |
| 3. | Breaking the plastic wave: a comprehensive assessment of pathways towards stopping ocean plastic pollution. Pew Charitable Trusts; 2020. |
| 4. | Dai L, Ruan R, You S, Lei H. Paths to sustainable plastic waste recycling. Science 2022; 377(6609): 934. doi: 10.1126/science.ade2221 |
| 5. | Lui G, Lai CKC, Chen Z, et al. SARS-CoV-2 RNA detection on disposable wooden chopsticks, Hong Kong. Emerg Infect Dis 2020; 26(9): 2274–6. doi: 10.3201/eid2609.202135 |
| 6. | Zhao W, van der Voet E, Huppes G, Zhang Y. Comparative life cycle assessments of incineration and non-incineration treatments for medical waste. Int J Life Cycle Assess 2009; 14(2): 114–21. doi: 10.1007/s11367-008-0049-1 |
| 7. | Bell L, Scutelnicu Todoran G. Plastic bag legislation in the United States: influential factors on its creation. J Environ Stud Sci 2022; 12: 260–71. doi: 10.1007/s13412-021-00736-8 |
| 8. | Hale RC, Song B. Single-use plastics and COVID-19: scientific evidence and environmental regulations. Environ Sci Technol 2020; 54(12): 7034–6. doi: 10.1021/acs.est.0c02269 |
| 9. | Repp KK, Keene WE. A point-source norovirus outbreak caused by exposure to fomites. J Infect Dis 2012; 205(11): 1639–41. doi: 10.1093/infdis/jis250 |
| 10. | Hirai Y. Survival of bacteria under dry conditions; from a viewpoint of nosocomial infection. J Hosp Infect 1991; 19(3): 191–200. doi: 10.1016/0195-6701(91)90223-U |
| 11. | Motz PDV, Young L, Motz M, Young S. A sticking point in assessing bacterial contamination: adhesive characters of bacterial specializations, swab features, and fomite surface properties skew colony counts. J Pure Appl Microbiol 2019; 13: 2533–44. doi: 10.22207/JPAM.13.4.68 |
| 12. | Takoi H, Fujita K, Hyodo H, et al. Acinetobacter baumannii can be transferred from contaminated nitrile examination gloves to polypropylene plastic surfaces. Am J Infect Control 2019; 47(10): 1171–5. doi: 10.1016/j.ajic.2019.04.009 |
| 13. | Kayes MI, Galante AJ, Stella NA, Haghanifar S, Shanks RMQ, Leu PW. Stable lotus leaf-inspired hierarchical, fluorinated polypropylene surfaces for reduced bacterial adhesion. React Funct Polym 2018; 128: 40–6. doi: 10.1016/j.reactfunctpolym.2018.04.013 |
| 14. | Lopez GU, Gerba CP, Tamimi AH, Kitajima M, Maxwell SL, Rose JB. Transfer efficiency of bacteria and viruses from porous and nonporous fomites to fingers under different relative humidity conditions. Appl Environ Microbiol 2013; 79(18): 5728–34. doi: 10.1128/AEM.01030-13 |
| 15. | Souli M, Galani I, Plachouras D, et al. Antimicrobial activity of copper surfaces against carbapenemase-producing contemporary Gram-negative clinical isolates. J Antimicrob Chemother 2013; 68(4): 852–7. doi: 10.1093/jac/dks473 |
| 16. | Wilks SA, Michels H, Keevil CW. The survival of Escherichia coli O157 on a range of metal surfaces. Int J Food Microbiol 2005; 105(3): 445–54. |
| 17. | Thormar H, Hilmarsson H. Killing of Campylobacter on contaminated plastic and wooden cutting boards by glycerol monocaprate (monocaprin). Lett Appl Microbiol 2010; 51(3): 319–24. doi: 10.1111/j.1472-765X.2010.02898.x |
| 18. | Gorman R, Bloomfield S, Adley CC. A study of cross-contamination of food-borne pathogens in the domestic kitchen in the Republic of Ireland. Int J Food Microbiol 2002; 76(1–2): 143–50. doi: 10.1016/S0168-1605(02)00028-4 |
| 19. | Mattick K, Durham K, Hendrix M, et al. The microbiological quality of washing-up water and the environment in domestic and commercial kitchens. J Appl Microbiol 2003; 94(5): 842–8. doi: 10.1046/j.1365-2672.2003.01904.x |
| 20. | Nerandzic MM, Thota P, Sankar CT, et al. Evaluation of a pulsed xenon ultraviolet disinfection system for reduction of healthcare-associated pathogens in hospital rooms. Infect Control Hosp Epidemiol 2015; 36(2): 192–7. doi: 10.1017/ice.2014.36 |
| 21. | Block C. The effect of Perasafe and sodium dichloroisocyanurate (NaDCC) against spores of Clostridium difficile and Bacillus atrophaeus on stainless steel and polyvinyl chloride surfaces. J Hosp Infect 2004; 57(2): 144–8. doi: 10.1016/j.jhin.2004.01.019 |
| 22. | Alqumber MA. Clostridium difficile in retail baskets, trolleys, conveyor belts, and plastic bags in Saudi Arabia. Saudi Med J 2014; 35(10): 1274–7. |
| 23. | Beumer, RR, Te Giffel, MC. Pathogens in domestic kitchens: facts and fiction. In: Tuijtelaars RA, Samson ACJ, Rombouts FM, Notermans S, eds. Food microbiology and food safety into the next millennium: Proceedings of the 17th international conference of the international committee on food microbiology and hygiene (ICFMH), Veldhoven, The Netherlands, 12-17 September 1999/Zeist: Foundation Food Micro, 1999, 99: 345–347. |
| 24. | Christison CA, Lindsay D, von Holy A. Cleaning and handling implements as potential reservoirs for bacterial contamination of some ready-to-eat foods in retail delicatessen environments. J Food Prot 2007; 70(12): 2878–83. doi: 10.4315/0362-028X-70.12.2878 |
| 25. | Sirsat SA, Choi JK, Almanza BA, Neal JA. Persistence of Salmonella and E. coli on the surface of restaurant menus. J Environ Health 2013; 75(7): 8–14; quiz 54. |
| 26. | Hayyan. I. Al-Taweil EMTNKMSYAD. Bacterial contamination of kitchen sponges and cutting surfaces and disinfection procedures. Indian J Public Health Res Dev 2020; 11(7): 1229–35. |
| 27. | Wendt C, Dietze B, Dietz E, Rüden H. Survival of Acinetobacter baumannii on dry surfaces. J Clin Microbiol 1997; 35(6): 1394–7. doi: 10.1128/jcm.35.6.1394-1397.1997 |
| 28. | Shimoda T, Okubo T, Enoeda Y, et al. Effect of thermal control of dry fomites on regulating the survival of human pathogenic bacteria responsible for nosocomial infections. J PLoS One 2019; 14(12): e0226952. |
| 29. | Allan JT, Yan Z, Genzlinger LL, Kornacki JL. Temperature and biological soil effects on the survival of selected foodborne pathogens on a mortar surface. J Food Prot 2004; 67(12): 2661–5. doi: 10.4315/0362-028X-67.12.2661 |
| 30. | Neely AN. A survey of gram-negative bacteria survival on hospital fabrics and plastics. J Burn Care Rehabil 2000; 21(6): 523–7. doi: 10.1097/00004630-200021060-00009 |
| 31. | Lücke F-K, Skowyrska A. Hygienic aspects of using wooden and plastic cutting boards, assessed in laboratory and small gastronomy units. J Verbrauchersch Lebensm 2015; 10: 317–22. doi: 10.1007/s00003-015-0949-5 |
| 32. | DeVere E, Purchase D. Effectiveness of domestic antibacterial products in decontaminating food contact surfaces. Food Microbiol 2007; 24(4): 425–30. doi: 10.1016/j.fm.2006.07.013 |
| 33. | Kim SJ, Si J, Lee JE, Ko G. Temperature and humidity influences on inactivation kinetics of enteric viruses on surfaces. Environ Sci Technol 2012; 46(24): 13303–10. |
| 34. | Takahashi H, Ohuchi A, Miya S, Izawa Y, Kimura B. Effect of food residues on norovirus survival on stainless steel surfaces. PLoS One 2011; 6(8): e21951. doi: 10.1371/journal.pone.0021951 |
| 35. | Fankem SL, Boone SA, Gaither M, Gerba CP. Outbreak of norovirus illness in a college summer camp: impact of cleaning on occurrence of norovirus on fomites. J Environ Health 2014; 76(8): 20–6. |
| 36. | Canales RA, Reynolds KA, Wilson AM, et al. Modeling the role of fomites in a norovirus outbreak. J Occup Environ Hyg 2019; 16(1): 16–26. doi: 10.1080/15459624.2018.1531131 |
| 37. | Mokhtari A, Jaykus LA. Quantitative exposure model for the transmission of norovirus in retail food preparation. Int J Food Microbiol 2009; 133(1–2): 38–47. |
| 38. | Mouchtouri VA, Koureas M, Kyritsi M, et al. Environmental contamination of SARS-CoV-2 on surfaces, air-conditioner and ventilation systems. Int J Hyg Environ Health 2020; 230: 113599. |
| 39. | Yang M, Li L, Huang T, et al. SARS-CoV-2 detected on environmental fomites for both asymptomatic and symptomatic patients with COVID-19. Am J Respir Crit Care Med 2021; 203(3): 374–8. doi: 10.1164/rccm.202006-2136LE |
| 40. | Ben-Shmuel A, Brosh-Nissimov T, Glinert I, et al. Detection and infectivity potential of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) environmental contamination in isolation units and quarantine facilities. Clin Microbiol Infect 2020; 26(12): 1658–62. doi: 10.1016/j.cmi.2020.09.004 |
| 41. | Geng Y, Wang Y. Stability and transmissibility of SARS-CoV-2 in the environment. J Med Virol 2023; 95(1): e28103. doi: 10.1002/jmv.28103 |
| 42. | Magurano F, Baggieri M, Marchi A, Rezza G, Nicoletti L. SARS-CoV-2 infection: the environmental endurance of the virus can be influenced by the increase of temperature. Clin Microbiol Infect 2021; 27(2): 289.e285–9.e287. doi: 10.1016/j.cmi.2020.10.034 |
| 43. | Riddell S, Goldie S, Hill A, Eagles D, Drew TW. The effect of temperature on persistence of SARS-CoV-2 on common surfaces. Virol J 2020; 17(1): 145. doi: 10.1186/s12985-020-01418-7 |
| 44. | Biryukov J, Boydston JA, Dunning RA, et al. Increasing temperature and relative humidity accelerates inactivation of SARS-CoV-2 on Surfaces. mSphere 2020; 5(4): 00441–00420. |
| 45. | Kasloff SB, Leung A, Strong JE, Funk D, Cutts T. Stability of SARS-CoV-2 on critical personal protective equipment. Sci Rep 2021; 11(1): 984. doi: 10.1038/s41598-020-80098-3 |
| 46. | Xie L, Liu F, Liu J, Zeng H. A nanomechanical study on deciphering the stickiness of SARS-CoV-2 on inanimate surfaces. ACS Appl Mater Interfaces 2020; 12(52): 58360–8. |
| 47. | Whitworth C, Mu Y, Houston H, et al. Persistence of bacteriophage Phi 6 on porous and nonporous surfaces and the potential for its use as an Ebola Virus or coronavirus surrogate. Appl Environ Microbiol 2020; 86(17): 1–11. doi: 10.1128/AEM.01482-20 |
| 48. | Bae SC, Park SY, Kim AN, Oh MH, Ha SD. Survival of hepatitis A virus on various food-contact surfaces during 28 days of storage at room temperature. Food Res Int 2014; 64: 849–54. |
| 49. | Thompson KA, Bennett AM. Persistence of influenza on surfaces. J Hosp Infect 2017; 95(2): 194–9. doi: 10.1016/j.jhin.2016.12.003 |
| 50. | Auger N, Rhéaume M-A, Bilodeau-Bertrand M, Tang T, Kosatsky T. Climate and the eye: case-crossover analysis of retinal detachment after exposure to ambient heat. Environ Res 2017; 157: 103–9. doi: 10.1016/j.envres.2017.05.017 |
| 51. | Abad FX, Pintó RM, Bosch A. Disinfection of human enteric viruses on fomites. FEMS Microbiol Lett 1997; 156(1): 107–11. doi: 10.1016/S0378-1097(97)00410-2 |
| 52. | Abad FX, Pintó RM, Bosch A. Survival of enteric viruses on environmental fomites. Appl Environ Microbiol 1994; 60(10): 3704–10. |
| 53. | Hall CB, Douglas RG, Jr, Geiman JM. Possible transmission by fomites of respiratory syncytial virus. J Infect Dis 1980; 141(1): 98–102. doi: 10.1093/infdis/141.1.98 |
| 54. | Sadowski R, Strus M, Buchalska M, Heczko PB, Macyk W. Visible light induced photocatalytic inactivation of bacteria by modified titanium dioxide films on organic polymers. Photochem Photobiol Sci 2015; 14(3): 514–9. doi: 10.1039/c4pp00270a |
| 55. | Livingston SH, Cadnum JL, Benner KJ, Donskey CJ. Efficacy of an ultraviolet-A lighting system for continuous decontamination of health care-associated pathogens on surfaces. Am J Infect Control 2020; 48(3): 337–9. doi: 10.1016/j.ajic.2019.08.003 |
| 56. | Mitchell JB, Sifuentes LY, Wissler A, Abd-Elmaksoud S, Lopez GU, Gerba CP. Modelling of ultraviolet light inactivation kinetics of methicillin-resistant Staphylococcus aureus, vancomycin-resistant Enterococcus, Clostridium difficile spores and murine norovirus on fomite surfaces. J Appl Microbiol 2019; 126(1): 58–67. |
| 57. | Bentley K, Dove BK, Parks SR, Walker JT, Bennett AM. Hydrogen peroxide vapour decontamination of surfaces artificially contaminated with norovirus surrogate feline calicivirus. J Hosp Infect 2012; 80(2): 116–21. doi: 10.1016/j.jhin.2011.10.010 |
| 58. | Rudnick SN, McDevitt JJ, First MW, Spengler JD. Inactivating influenza viruses on surfaces using hydrogen peroxide or triethylene glycol at low vapor concentrations. Am J Infect Control 2009; 37(10): 813–9. |
| 59. | Yeargin T, Fraser A, Huang G, Jiang X. Recovery and disinfection of two human norovirus surrogates, feline calicivirus and murine norovirus, from hard nonporous and soft porous surfaces. J Food Protect 2015; 78(10): 1842–50. doi: 10.4315/0362-028X.JFP-14-515 |
| 60. | Sexton JD, Wilson AM, Sassi HP, Reynolds KA. Tracking and controlling soft surface contamination in health care settings. Am J Infect Control 2018; 46(1): 39–43. doi: 10.1016/j.ajic.2017.08.002 |
| 61. | Beer D, Vandermeer B, Brosnikoff C, Shokoples S, Rennie R, Forgie S. Bacterial contamination of health care workers’ pagers and the efficacy of various disinfecting agents. Pediatr Infect Dis J 2006; 25(11): 1074–5. doi: 10.1097/01.inf.0000242649.27400.94 |
| 62. | Gaunt L, Higgins S, Hughes J. Decontamination of surface borne bacteria by ionized antimicrobial vapours. J Electrostat 2005; 63(6): 809–14. doi: 10.1016/j.elstat.2005.03.076 |
| 63. | Demir B, Broughton R, Huang T, Bozack M, Worley S. Polymeric antimicrobial N-halamine-surface modification of stainless steel. Ind Eng Chem Res 2017; 56: 11773–81. doi: 10.1021/acs.iecr.7b02412 |
| 64. | Sharma M, Hudson JB. Ozone gas is an effective and practical antibacterial agent. Am J Infect Control 2008; 36(8): 559–63. doi: 10.1016/j.ajic.2007.10.021 |
| 65. | Rupp ME, Huerta T, Yu S, et al. Hospital basins used to administer chlorhexidine baths are unlikely microbial reservoirs. Infect Control Hosp Epidemiol 2013; 34(6): 643–5. doi: 10.1086/670622 |
| 66. | Thormar H, Hilmarsson H. Glycerol monocaprate (monocaprin) reduces contamination by Escherichia coli and Salmonella enteritidis on hard surfaces. Food Control 2012; 25(2): 505–10. doi: 10.1016/j.foodcont.2011.11.024 |
Appendices
Ovid MEDLINE Search Conducted October 10, 2021
- (Bamboo or Plastic or Cloth or cotton or hemp or Composite materials or glass or polyethylene or Molded fiber or Polypropylene or Polystyrene or Styrofoam or foodware or utensils or steel or metal or cardboard or ((coated or treated or wax) adj2 paper)).ti,ab.
- (Coronaviruses or Deltacoronavirus or Betacoronavirus or 2019-nCoV or covid or Staphylococcus or Norovirus or E. coli or Escherichia coli or Campylobacter or Salmonella or Clostridium or Listeria).mp. [mp=title, abstract, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword, floating subheading word, candidate term word]
- 1 and 2
- transfer efficiency.ti,ab.
- exp Cross Infection/
- fomites.mp. or exp Fomites/
- (Microbial adj2 viab*).ti,ab.
- 4 or 5 or 6 or 7
- 3 and 8
- exp *Viruses/
- 1 and 8 and 10
- exp *Fomites/
- 9 or 11 or 12
- fomite*.mp. or exp Fomites/
- 8 or 14
- 1 and 2 and 15
- 13 or 16
Summary of Included Studies
| Pathogens | Count of included papers | Disinfection study | Lab-based (ex: Anything using surrogates, taking material and applying pathogen to it) | In-Situ (Case study or live setting) | Modeling | Lab-based + Disinfection | In-Situ + Disinfection | Modeling + Disinfection |
| SARS-CoV-2 (Covid 19) | 13 | 2 | 10 | 4 | 0 | 1 | 1 | 0 |
| Campylobacter spp. | 3 | 2 | 2 | 1 | 0 | 2 | 0 | 0 |
| Listeria | 3 | 0 | 1 | 2 | 0 | 0 | 0 | 0 |
| GENERAL viral/respiratory (i.e. flu, etc.) | 14 | 3 | 12 | 2 | 1 | 2 | 1 | 0 |
| Salmonella spp. | 15 | 3 | 12 | 5 | 0 | 3 | 1 | 0 |
| Clostridium perfringen/ C. diff | 10 | 8 | 7 | 4 | 2 | 6 | 3 | 2 |
| Norovirus | 31 | 11 | 23 | 7 | 3 | 9 | 2 | 1 |
| GENERAL bacteria (i.e. gram negative or gram positive); should not include bacteria that form spores (Bacillus) | 42 | 14 | 31 | 14 | 1 | 10 | 7 | 1 |
| E. coli | 48 | 15 | 41 | 12 | 2 | 14 | 4 | 0 |
| TOTAL | 179 | 58 | 139 | 51 | 9 | 47 | 19 | 4 |