ORIGINAL ARTICLE
Australia’s states and territories Infection Prevention and Control programs – a comparison study
Kathy Dempsey1*, Susan Jain2, Patricia Bradd3, Kate Clezy4 and David Greenfield5
1NSW Chief Infection Prevention and Control Practitioner and Healthcare Associated Infection Advisor, Clinical Excellence Commission, University of NSW, Sydney, Australia; 2Principal Advisor and Research Lead Infection Prevention and Control and Healthcare Associated Infection, Sydney, Australia; 3Director Patient Safety, Sydney, Australia; 4Medical Advisor Infection Prevention and Control and Healthcare Associated Infection, Sydney, Australia; 5Professor of Health Leadership, School of Population Health, UNSW Medicine, Sydney, Australia
Abstract
Background: Infection prevention and control (IPC) remains a critical component of delivering quality and safe care. However, clinician understanding of and engagement with IPC remain inconsistent (1–3). In addition, IPC governance, structure and organisation impact on clinician engagement are not well described. Available publications are limited to healthcare-associated infection (HAI) surveillance and do not reflect the broader IPC program (4–6). As Australia establishes a national coordinating body similar to a Centers for Disease Control and Prevention (CDC), a comparison of jurisdictional IPC provides essential contemporary information to inform the national body.
Method: This study examined the characteristics of jurisdictional (states and territories) IPC programs in Australia and was conducted in two phases. Phase one examined outward facing websites likely to be accessed by clinicians, and phase two surveyed jurisdictional programs using a qualitative questionnaire.
Results: Whilst each jurisdiction had accessible website content, this varied considerably in terms of governance, structure, content, ease of navigation, accessibility and visibility. There was a lack of national focus within jurisdictional programs and websites. Four of eight jurisdictions did not have a formal statewide IPC program at the time of the survey. Variance was reported in governance, structures, focus and program elements.
Conclusion: Inconsistent IPC governance and structure demonstrates poorly aligned Australian IPC programs that may contribute to poor clinician understanding and engagement with IPC. Implementing a coordinated and consistent approach to governance, website design and layout would facilitate a consolidated approach to IPC nationally, which may facilitate clinician understanding and engagement. Shaping IPC nationally would also provide solid IPC foundations to support an Australian CDC.
Keywords: infection prevention and control; Healthcare-associated infection; Infection prevention and control practitioner; Clinicians – Health workers including physicians involved in delivery and support of patient care
Citation: Int J Infect Control 2024, 20: 23444 – http://dx.doi.org/10.3396/ijic.v20.23444
Copyright: © 2024 Kathy Dempsey et al. This is an Open Access article distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for any purpose, even commercially, provided the original work is properly cited and states its license.
Received: 5 March 2023; Accepted: 13 March 2024; Published: 21 May 2024.
Competing interests and funding: The authors declare no conflict of interest. No funding was received in relation to this work.
*Kathy Dempsey, Clinical Excellence Commission, NSW Health., 1 Reserve Road St Leonards NSW 2065, Locked Bag 2030, St Leonards NSW 1590, Australia. Email: Kathy.dempsey@health.nsw.gov.au
Understanding and comparing structures and governance for healthcare-associated infections (HAIs) and infection prevention and control (IPC) programs across Australia provides a current roadmap and informs future pathways. This study investigates Australian state and territories (jurisdictional) program structures and governance of IPC programs. It examines both the consistency and variability in program design, structure, governance and accessibility of IPC information for clinicians. Given the study was conducted part way through the COVID-19 pandemic and the assumed IPC leadership role, the jurisdictional programs would play information about IPC programs, and pandemic function was also collected.
This knowledge is useful to inform Australian Government’s decision-making in establishing a national IPC framework for a new national body, an Australian Centre for Disease Control (CDC).
Background
IPC programs are a major contributor to quality and safety and provide access to HAI data, a key indicator of patient safety success or failures (7). The COVID-19 pandemic raised the visibility and focus on IPC programs – from governments, clinicians and the community, far surpassing any previous attention. Consistent and reliable communication with widespread dissemination of IPC guidelines was the norm for the last 3 years, including strategies that drive IPC program compliance (8–10). Even with this unprecedented attention, clinician understanding and engagement with IPC programs did not improve substantially (8).
The challenge of improving clinician engagement is longstanding (11). The World Health Organisation (WHO) IPC program recommendations identify eight core components relevant for national and facility level programs. These include IPC guidelines; implementation strategies; monitoring, auditing and feedback mechanisms; education and training policies; HAI surveillance; facility level human resource management directions; and built environment and equipment requirements for IPC (11, 12). However, the effective implementation of these recommendations across many countries remains inconsistent, with inadequate programs resulting in low-quality care and ongoing and increased risk of harm (11). Unsurprisingly, barriers to IPC program implementation mirror these requirements, including inadequate guideline development, release timing, and communication between stakeholders and resourcing (8). The result being that, in many countries, HAIs continue to significantly impact individual patients and consume health resources (4, 13, 14). The growing evidence for and the development of core components for IPC programs have not resulted in an effective interconnected national and jurisdictionally embedded system for many countries including Australia (10, 11, 15, 16). Australia’s ability to implement WHO guidelines is likely to be further compounded by inconsistent governance and structures to jurisdictional programs and lack of connecting national program.
Whilst facing problems of IPC common to other countries, Australia has some particular issues. The Australian health system’s resourcing, governance and service delivery is highly complex and distributed (17). Australia is a federation with a national bureaucracy, and six States and two Territories, each with an independent jurisdictional department of health. The national department of health interacts and coordinates policy and funding arrangements with the states and territories. In 2023, each jurisdiction is required to have a HAI program supported by the national agency, the Australian Commission on Safety and Quality in Health Care (ACSQHC) (18). The current arrangements emerged from Australia’s long history of IPC programs dating back to the 1940/1950s, when outbreaks of hospital-associated infections were first described and investigated (19). The longitudinal development and implementation of how to govern this work was largely uncoordinated and left to each jurisdiction to determine. Today, jurisdictional IPC programs support their health organisations through separate arrangement, including resourcing, policies and procedures, HAI management and facility-based IPC practitioners. Each jurisdiction has responsibility to implement IPC strategies locally, such as HAI surveillance; hand hygiene; outbreak management; multidrug resistant organism surveillance and management; environmental cleaning; reprocessing of reusable medical equipment; health infrastructure; education and training; and antimicrobial stewardship (AMS) programs (18, 20).
In Australia, there is no nationally coordinated IPC program. Historically, separate jurisdictional IPC programs were established to promote patent safety and reduce HAIs; (21–24) hence, they were referred to as HAI programs. This naming has contributed to a lack of understanding and engagement by clinicians regarding other IPC program elements (25). A further challenge is that there has not been investigation, analysis nor agreement on the structure and resourcing for IPC programs. This has led to a disconnect between jurisdictional IPC programs and clinicians delivering care, whereby clinicians view them as high-level governance systems unrelated to their patient care delivery (26).
There is a major knowledge gap on the impact of national and state level IPC programs and the elements of large-scale jurisdictional programs, within Australia and across other countries. Effective planning for future pandemics necessitates this knowledge gap to be filled. Hence, the aim of this study was to investigate Australian IPC programs governance and structure arrangements, program elements, compliance with the WHO IPC program core components and role in COVID-19 IPC response.
Methods
Setting
The study setting was the six states and two territories in the Australian health system. Additionally, the ACSQHC, the key national agency associated with HAI programs, was included.
Study ethics approval and phases
Ethics approval was obtained from the Northern Sydney Local Health District (NSLHD) ethics committee and endorsed for each jurisdiction (2021/ETH01203). This study was conducted in two sequential phases.
Phase one: website search
An internet search focusing on program governance, structure, program elements and COVID-19 response was conducted to determine the visibility and accessibility of jurisdictional IPC or HAI program information for clinicians. The search involved an internet keyword search linking the jurisdiction and topic, for example ‘Queensland and HAI program’ or ‘South Australia infection control’. Websites were also searched for role and information relating to IPC and COVID-19. Combinations such as these identified webpages associated with programs at departments of health at the state and territory levels. Governance was assessed via organisational charts and reporting lines visible on the website. The task was completed in 2021.
Framework analysis with a deductive semantic approach was used to analyse the information (27). This is an approach suitable for policy research with homogenous data, which creates a matrix of summarised material. The categories of information were predefined and used to identify the explicit content in the websites. Content headings included the following: the responsible program agency; program title; governance structure; associated information, factsheets or guidelines; education and training materials; and if the jurisdictional website was the repository for COVID-19 IPC resources.
Phase two: online survey
Phase two was an online survey with participants from the jurisdictional programs and ACSQHC. The survey was piloted and validated by an expert volunteer advisory panel, randomly selected, that included representation from senior IPC practitioners and policy makers. The survey, comprising 26 open, closed and free text questions (Appendix 1: Survey), investigated IPC program governance – reporting lines, structure – staffing numbers, program elements, ICP experience and if jurisdictional program also led IPC COVID-19 response and resources allocated. Jurisdictional staff were invited by email to participate. They received the study protocol, ethics approval, instructions and the survey QR code link. It was anticipated that the survey would take approximately 20 min to complete. The survey was conducted from July to September 2021. Emails were sent to two nominated contacts of each jurisdiction and the ACSQHC, and surveys were completed to reflect the nature of IPC for the respective jurisdiction. Multiple participants from each jurisdiction and the ACSQHC provided a response; in total, 17 individual surveys were returned representing a response from all eight jurisdictions and the ACSQHC, reflecting the distributed leadership for IPC and HAI programs. Survey responses were exported from Microsoft Forms into Microsoft Excel for cleaning and validation. Responses of program elements were sorted to align with the WHO IPC core components. Responses then were themed and sorted. Thematic analysis and the Cross-tabulation method were used to analyse the data and draw conclusions (27).
Results
The results for phases one and two are presented in order.
Phase one: website search
IPC and/or HAI subject matter were identified for the eight jurisdictions and the national agency, the ACSQHC (Table 1). Each site presented either as a focused comprehensive named program or a component within another, with different structures and format and with no consistency between them. Variance in governance and the operating frameworks was found between the jurisdictions. IPC programs were governed either under a patient safety framework or as an arm of public health, such as communicable diseases or health protection. Leadership role relating to IPC and COVID-19 also varied.
| NSW | WA | SA | TAS | VIC | QLD | ACT | NT | ACSQHC | ||
| Agency | Clinical Excellence Commission NSW Health |
Department of Health | SA Health | Department of Health | Safer Care Victoria | QLD Health | ACT Health | Department of Health | Australian Commission on Safety and Quality in Health care | |
| Website | www.cec.health.nsw.gov.au | www.health.wa.gov.au | www.sahealth.sa.gov.au | www.health.tas.gov.au | www2.health.vic.gov.au www/dhhs.vic.gov.au |
www.qld.gov.au clinicalexcellence.qld.gov.au |
www.health.act.gov.au | www.safetyandquality.gov.au | www.safetyandquality.gov.au | |
| PROGRAM TITLE | Infection Prevention and Control and HAI program | Communicable disease control: healthcare-associated infections | SA Health Infection Control Service | Infection Prevention and Control | Healthcare-associated infection prevention | 1. Healthcare-associated infection. 2. Infection Prevention |
Infection Prevention and Control | Infection Management | Healthcare-Associated Infection Program | N = 9 |
| Combined IPC and HAI Focus | ✓ | ✓ | ✓ | ✓ | N = 4 | |||||
| IPC PRIMARY FOCUS | ✓ | N = 3 | ||||||||
| HAI PRIMARY FOCUS | ✓ | ✓ | ✓ | N = 3 | ||||||
| Accessible Resources | ✓ | ✓ | ✓ | ✓ | ✓ | N = 5 | ||||
| COVID-19 IPC Lead | ✓ | ✓ | ✓ | N = 3 | ||||||
| GOVERNANCE | ||||||||||
| Patient Safety | ✓ | ✓ | ✓ | N = 3 | ||||||
| Public Health/Communicable Disease | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | N = 6 | |||
 Not located on website as being part of program ✓ = information located Resources include Guidelines, factsheets, posters, toolkits, education and training materials Not located on website as being part of program ✓ = information located Resources include Guidelines, factsheets, posters, toolkits, education and training materials |
||||||||||
| NSW, New South Wales; WA, Western Australia; SA, South Australia; TAS, Tasmania; Vic, Victoria; QLD, Queensland; ACT, Australian Capital Territory; NT, Northern Territory; ACSQHC, Australian Commission on Safety and Quality in Healthcare. | ||||||||||
| NB: Jurisdictions that did not have a jurisdictional program had HAI monitoring in isolation under different governance. | ||||||||||
Three of eight jurisdictions displayed a structured web-based IPC framework responsible for IPC, HAI and as the repository for COVID-19 IPC resources, that is New South Wales (NSW), South Australia (SA) and Western Australia (WA). The remaining five – Queensland (QLD), Australian Capital Territory (ACT), Northern Territory (NT), Victoria (VIC) and Tasmania (TAS) – focused on HAI only with no statewide IPC program displayed. The national agency, the ACSQHC, operates under a patient safety framework with a focus on preventing and controlling HAIs, rather than an IPC program. Governance relating to IPC and COVID-19 was less clear in nearly all jurisdictional program websites. The ACSQHC was not the lead Australian IPC agency for COVID-19; instead, a newly formed group was created – the National Infection Control Expert Group (ICEG) – during the pandemic consisting of experts in infectious diseases and IPC. There appeared to be little interconnection across jurisdictional websites for the ACSQHC, ICEG and the Australian Department of Health.
Table 1 provides detailed responses relating to the website comparison across Australia.
Phase two: online survey
Phase two further explored the characteristics and core components of HAI programs in jurisdictions and their focus (if any) on IPC. The survey confirmed findings from Phase one relating to variable governance, structure and program components.
Infection prevention and control practitioner (ICP) experience was reported spanning 6 to 32 years across the jurisdictions. However, the line of questioning was limited to length of time as an ICP and did not explore the context, experience or the type of experience of the ICP in any detail. Years in the state role were between 0 and 25 years. Five of eight programs plus the ACSQHC reported being led by an ICP, and interestingly, only two of those reported being credentialled experts. Teams across each state and territory reported between 1.6 Fulltime Equivalent (FTE) and 12 FTE staff with the majority having reported a temporary increase in staff numbers to their program in response to COVID-19.
As part of program structure, jurisdictional program names varied from HAI Program, Infection Management, HAI and IPC to Infection Prevention and Control Advice and Response (COVID-19 only). Half of the jurisdictions (4 of 8) reported not having a recognised named jurisdictional IPC or HAI program (Figure 1: Jurisdictional HAI and IPC Program distribution). Jurisdictional programs that were specific to HAI/IPC were better aligned to the ACSQHC via published program elements and consistently demonstrated compliance to the Australian National Safety and Quality Health Services Standards (NSQHSS) for accreditation of IPC (7). When aligned with WHO core components of IPC, however, no individual program throughout Australia demonstrated full compliance. Jurisdictions who reported having an IPC program, NSW, WA, SA and TAS, reported both a HAI and IPC focus. Those jurisdictions reporting no statewide programs – VIC, QLD, ACT and NT – described a public health focus inclusive of HAI. One jurisdiction – VIC – describes no statewide program but responsibility for HAI surveillance aligned to an external agency to the health department and public health and was not involved in IPC during COVID-19. The four jurisdictions reporting no statewide HAI/IPC program (VIC, QLD, ACT and NT) reported a preference to have such a program.
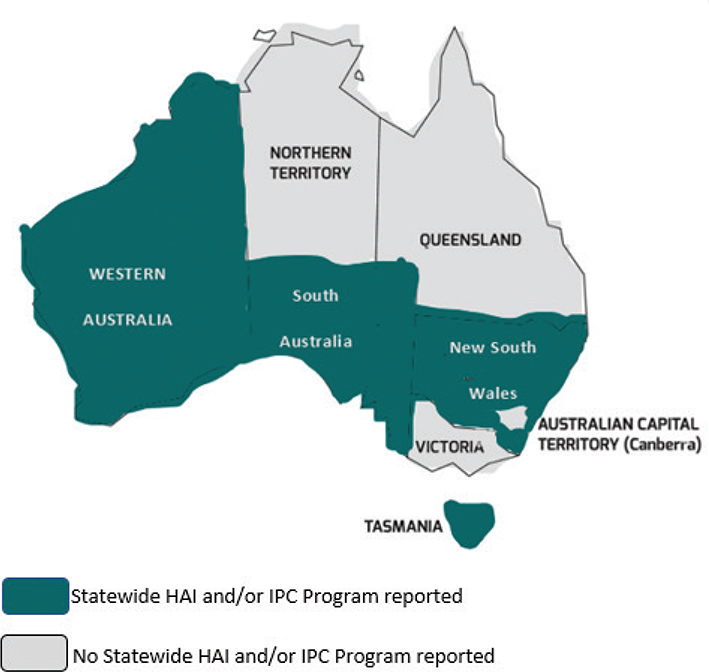
Fig. 1. Jurisdictional HAI and IPC program distribution.
NB: Jurisdictions with no jurisdictional program reported inclusion of HAI as a project of public health without a statewide program.
In Australia during the ongoing COVID-19 pandemic, additional governance frameworks for IPC emerged within jurisdictions. Three of the eight jurisdictions, NSW, WA and SA, functioned as the lead agency for IPC response during the COVID-19 pandemic. The remaining five plus the ACSQHC did not have a role, and their jurisdiction created alternative and very separate governance structures.
The survey explored the characteristics required for a statewide run program with the following consistently cited across all jurisdictions: Statewide and national HAI surveillance and data system, adequate and suitable resourcing, and IPC expertise and effective leadership. Whilst the program elements were consistent as seen in Table 2, when programs were compared to the WHO IPC core components (Table 3 WHO IPC Core Components and Australia’s Jurisdictional Programs Compliance), this resulted in an overall poor report card for Australian IPC.
Clinicians supported by the jurisdiction were most likely not aware that HAI programs were also responsible for IPC more broadly (Figure 2). According to respondents, the structures for HAI/IPC programs likely affected the preparedness of IPC response to COVID-19 pandemic (Figure 3).
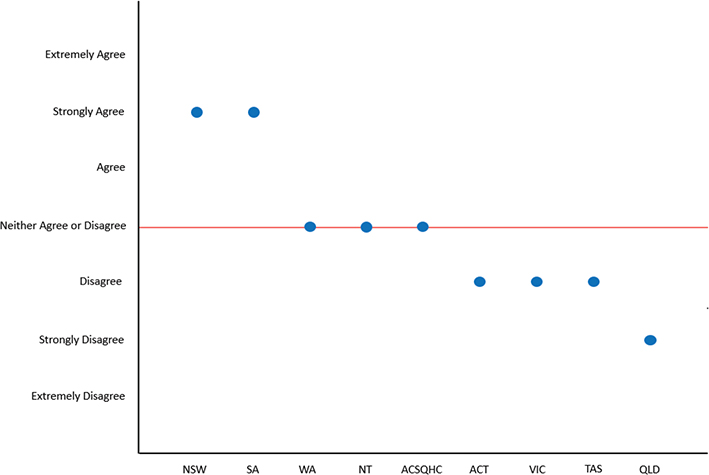
Fig. 2. The health system and the clinicians. The jurisdictional program supports understanding the statewide HAI program also leads IPAC.
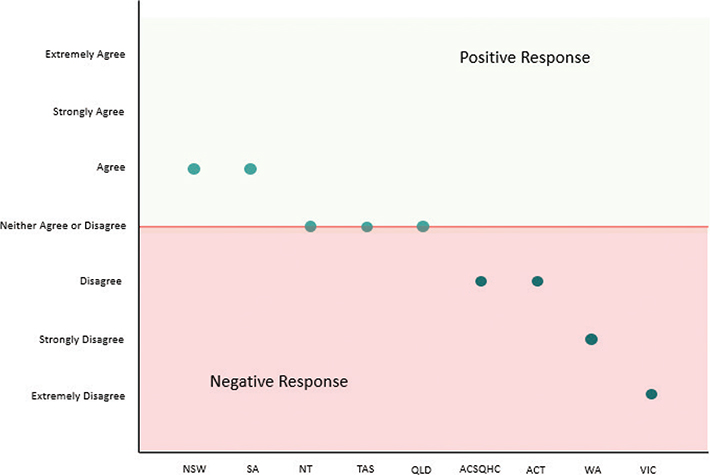
Fig. 3. The structure for state/territory HAI/IPAC programs enabled a well-prepared response to COVID-19 pandemic.
Discussion
Our study provides an in-depth understanding of IPC programs across Australian jurisdictions making explicit reference to multiple issues and process gaps. A search of websites showed information and resources were available but varied in comprehensiveness. Although each jurisdictional program website showed commitment to IPC and HAI prevention, there is lack of clear governance, consistency in resources and themes and clear link or collaboration between any of the jurisdictions or nationally to the ACSQHC site.
The website search identified often complex and confusing pathways to navigate sites that would likely impact clinicians’ ability to comprehend or find necessary resources. However, it was difficult to navigate and describe the variability and complexities of navigating websites. This may be considered as a contributing factor to the lack of clinician understanding of IPC governance, structures, program elements, core components, resources and implementation of IPC. A recent paper by Baswa et al., which looked at barriers to IPC, specifically focused on COVID-19 barriers to the implementation of IPC guidance from government authorities such as those responsible for jurisdictional HAI and IPC programs and highlighted communication as a key barrier (8). Baswa’s study, however, focuses on local facilities rather than state or national level programs, which also differs from the primary focus of the WHO global survey. The complex structures of state and national level programs are likely to be contributing to poor clinician engagement as clinicians would require specific knowledge and information to navigate access to resources.
The WHO global survey (2019) highlighted the need for increased support for more effective and sustainable IPC programs as crucial to reduce risks posed by outbreaks to global health security and to ensure patient’s and health worker’s safety (11). Given the criticality of these IPC systems, understanding Australia’s jurisdictional and national IPC programs is an important consideration of IPC particularly considering an Australian CDC is being established.
Workforce optimisation is a vital component in effective delivery of any IPC program and necessary to reduce the global burden of disease related to HAI. Yet, it remains an area of debate, and limitations (28) also illustrated in this Australian comparison study. A major gap of the WHO core components and global survey is the translatability beyond local facility implementation to jurisdictional or national program requirements. Translating findings of the WHO global survey to jurisdictional or national IPC programs would require similar structures, functions and resources to drive impact and change across Australia. Consistent with WHO findings, few jurisdictions were able to demonstrate compliance with all WHO core components, particularly those with no recognised jurisdictional program in place (11).
Only two jurisdictional programs demonstrated leadership of their program by credentialled expert ICPs. Credentialling in Australia provides a clear industry-recognised pathway, whereby the necessary knowledge, skills and attributes is recognised by expert peers as a Primary, Advanced or Expert credentialled infection Control Professional (29, 30). This level of experience is usually associated with better outcomes; however, further study in this area would be useful (29, 30).
Our study showed navigating jurisdictional websites for HAI or IPC was challenging, with inconsistent and variable public information, content variability and available resources having poor to no alignment to the ACSQHC as the recognised Australian national accreditation body for HAI and IPC. HAI governance and program characteristics (core components) in Australia were varied with some not reported at all.
Responsibility for the coordination of infection control programs in Australia was first studied by Murphy and McLaws who highlighted the need for standardisation in practice and surveillance, training and ongoing education and encouragement of research initiatives (16). However, more than two decades, standardisation has not been achieved across IPC programs. The pilot study by Shaban et al. (29) of two Australian jurisdictions examined the documentation, composition and organisation of IPC programs at an institutional level rather than statewide governing programs. This work facilitated a conceptual shift from commonly held, traditional understandings and approaches to IPC program strategies that align with constructivist theories of active engagement of clinicians with a more structured approach. This suggests the need for a structured well defined and consistent approach to jurisdictional and national IPC programs. Our study further supports that, without clear and well-defined structures and governance differences, clinicians may not access necessary information and responses to IPC are more likely to be negative (Figure 2). The existing IPC programs (and the lack of programs) also elicited a mostly negative response for enabling a well-prepared IPC for COVID-19 pandemic (Figure 3). This variability further suggests a disconnect between COVID-19 IPC and in some existing jurisdictional HAI/IPC programs. This variability in governance for IPC compounds the difficulties with understanding by clinicians and the system more broadly of governance for IPC (8). Global IPC priorities call for strengthened IPC visibility, advocacy and elevation of the role, requiring strong empowerment and support from national leaders in acknowledgement of the value of IPC (12, 30, 31). A challenge for IPC success is that it is often measured on outcomes relating to the reduction of HAIs, whereas the burden of work centres around many other aspects rarely reported. The few reported studies that exist show that the burden of work for IPC is most likely centred around: outbreak management and risk assessment strategies; problem solving and critical thinking; managing IPC breaches; education and training of staff (32–34). These factors are most likely important for changing behaviour of clinicians to drive compliance (33, 34). Acknowledging these diverse range of issues around IPC and patient and staff safety is critical.
The historical function and structure of Australian HAI programs at a jurisdictional and national levels may be contributing to the lack of engagement and understanding of IPC by clinicians. Many IPC programs are under resourced when compared with the staffing levels recommended in the literature of 1.0 (FTE) ICP per 250 beds and 1.0 (FTE) ICP for every 100 overnight acute care beds. Whilst not specifically quantified in this study, there is variation in staff numbers, structure, experience, credentialling and competency correlating to both quality and implementation capacity of the jurisdictional programs within Australia (12, 20, 35–41).
Moving to a consistent national framework which includes surveillance systems and other tools to facilitate an efficient and effective program that is easy for clinicians to navigate is critical to advance the effectiveness of IPC (thereby improving patient safety). This in turn would lead to better engagement of clinicians resulting in greater understanding and implementation of IPC. The interim Australian CDC is lacking in IPC but rather looks to the existing national and jurisdictional programs demonstrated here as inconsistent. Several countries are supported by Centres for Disease Control and Prevention or similar. This includes the United States, European Union and Central Asia, who have a national approach to manage and guide IPC. Based on our findings, other countries may also look to their own program approach nationally, program governance and structure to improve clinician engagement and safe care provision.
Despite many individual and well-structured jurisdictional programs, this study shows that Australia may benefit from improved organisational consistency and high-level intelligence in the development of an Australian CDC (30). Continued discussions and evolution of an Australian CDC would require collaboration with those most experienced at IPC and greater involvement with any future directions. Furthermore, comprehensive infectious diseases surveillance and real time data analysis would be critical for coordinating a national disease control response, requiring an experienced workforce with expertise in epidemiology, microbiology, public health and IPC (30). This would assist to reduce the significant gaps occurring across jurisdictions and national programs. Improved structure and consistency may improve confidence and credibility in the system.
To enhance IPC across the country, the future direction for IPC programs across Australia and globally should have robust and solid foundations that enhance connection with clinicians and key experts and improved consistency and instil a higher level of confidence.
Limitations
The quality of the evidence has some limitations related to the utilisation of self-reported survey method. However, there was a 100% response rate, as each state and territory provided a response. The website search was limited to external facing sites. Several changes to websites may have occurred following searches and during the study period in response to COVID-19 in the rapidly changing IPC environment. The line of enquiry for IPC experience may be limited as it did not differentiate whether experience was frontline IPC or policy related. This study represents a high-level comparison of IPC programs across Australia but would benefit from analysis of clinicians’ insight to these programs directly and a level of evaluation of programs. The time period of this study, overwhelming workloads and rapidly evolving IPC systems during and in response to the COVID-19 pandemic also saw several changes occurred during the study period that may have affected the findings.
Conclusion
Limited research on the effectiveness and essential elements of Australian IPC jurisdictional programs continues to be a gap in the literature. As shown by the WHO’s first global survey on IPC in healthcare facilities, further investments are needed for effective implementation of IPC training programs. Our research has provided a comparison across Australia to inform and facilitate a way forward and insights for consideration as Australia navigates its own CDC. Additional research is also required to ensure programs responsible at government level utilise a consistent national and statewide approach to IPC to better position and embed them into patient safety pathways and build a scalable IPC system to foster clinician engagement with IPC programs.
Acknowledgement
The authors thank the contributing members from the jurisdictional programs and the key stakeholder group for their contribution during extremely busy times. The information in this article does not assess the effectiveness of the jurisdictional programs nor reflect the work being done as part of these programs and acknowledges the IPC contributions by each of the jurisdictions and the efforts by all ICPs.
The authors would also like to acknowledge, in memory, two remarkable individuals as original researchers and supervisors in this work. We dedicate this acknowledgement with profound gratitude and heartfelt appreciation to Prof Mary-Louise McLaws (AO) (Dec) and Dr Annette Pantle (AM) (Dec).
Ethical approval
Ethics approval was obtained from the Human Research Ethics Committee of Northern Sydney Local Health District (NSLHD) and was granted ethical and scientific approval of multi-centre project: 2021/ETH01203. The HREC were satisfied that this project met the requirements of the National Statement. This project was approved to be conducted at the following sites:
- Australian Commission Quality and Safety in Health Care – HAI Jurisdictional Steering Committee
- New South Wales Health
- Victoria Health
- Queensland Health
- Western Australia Health
- South Australia Health
- Tasmania Health
- Australian Capital Territory Health
- Northern Territory Health
Disclosure statement
The authors declare no potential conflicts of interest with respect to the research authorship and/or publication of this article.
References
| 1. | Kim H, Hwang YH. Factors contributing to clinical nurse compliance with infection prevention and control practices: a cross-sectional study. Nurs Health Sci 2020; 22(1): 126–33. doi: 10.1111/nhs.12659 |
| 2. | Cole M. Compliance and infection control guidelines: a complex phenomenon. Br J Nurs 2008; 17(11): 700–4. doi: 10.12968/bjon.2008.17.11.29615 |
| 3. | Gilbert GL, Kerridge I. The politics and ethics of hospital infection prevention and control: a qualitative case study of senior clinicians’ perceptions of professional and cultural factors that influence doctors’ attitudes and practices in a large Australian hospital. BMC Health Serv Res 2019; 19(1): 1–10. doi: 10.1186/s12913-019-4044-y |
| 4. | Russo PL, Cheng AC, Richards M, Graves N, Hall L. Healthcare-associated infections in Australia: time for national surveillance. Aust Health Rev 2014; 39(1): 37–43. doi: 10.1071/AH14037 |
| 5. | Mitchell BG, Shaban RZ, MacBeth D, Wood C-J, Russo PL. The burden of healthcare-associated infection in Australian hospitals: a systematic review of the literature. Infect Dis Health 2017; 22(3): 117–28. doi: 10.1016/j.idh.2017.07.001 |
| 6. | Russo PL, Cheng AC, Richards M, Graves N, Hall L. Variation in health care-associated infection surveillance practices in Australia. Am J Infect Contr 2015; 43(7): 773–5. doi: 10.1016/j.ajic.2015.02.029 |
| 7. | Stewart S, Robertson C, Pan J, Kennedy S, Dancer S, Haahr L, et al. Epidemiology of healthcare-associated infection reported from a hospital-wide incidence study: considerations for infection prevention and control planning. J Hosp Infect 2021; 114: 10–22. doi: 10.1016/j.jhin.2021.03.031 |
| 8. | Baswa A, Russo PL, Doyle JS, Ayton D, Stewardson AJ. Experience and perspectives of infection prevention staff of the COVID-19 response in Australian hospitals. Antimicrob Resist Infect Contr. 2022; 11(1): 77. doi: 10.1186/s13756-022-01116-9 |
| 9. | Lowe H, Woodd S, Lange IL, Janjanin S, Barnet J, Graham W. Challenges and opportunities for infection prevention and control in hospitals in conflict-affected settings: a qualitative study. Conflict Health 2021; 15(1): 1–10. doi: 10.1186/s13031-021-00428-8 |
| 10. | Houghton C, Meskell P, Delaney H, Smalle M, Glenton C, Booth A, et al. Barriers and facilitators to healthcare workers’ adherence with infection prevention and control (IPC) guidelines for respiratory infectious diseases: a rapid qualitative evidence synthesis. Cochrane Database Syst Rev 2020; 4: CD013582. doi: 10.1002/14651858.CD013582 |
| 11. | Tomczyk S, Twyman A, de Kraker ME, Rehse APC, Tartari E, Toledo JP, et al. The first WHO global survey on infection prevention and control in health-care facilities. Lancet Infect Dis 2022; 22(6): 845–56. doi: 10.1016/S1473-3099(21)00809-4 |
| 12. | Storr J, Twyman A, Zingg W, Damani N, Kilpatrick C, Reilly J, et al. Core components for effective infection prevention and control programmes: new WHO evidence-based recommendations. Antimicrob Resist Infect Contr 2017; 6: 1–18. doi: 10.1186/s13756-016-0149-9 |
| 13. | Russo PL, Havers SM, Cheng AC, Richards M, Graves N, Hall L. Characteristics of national and statewide health care–associated infection surveillance programs: a qualitative study. Am J Infect Contr 2016; 44(12): 1505–10. doi: 10.1016/j.ajic.2016.06.034 |
| 14. | Gesser-Edelsburg A, Cohen R, Halavi AM, Zemach M, van Heerden PV, Sviri S, et al. Beyond the hospital infection control guidelines: a qualitative study using positive deviance to characterize gray areas and to achieve efficacy and clarity in the prevention of healthcare-associated infections. Antimicrob Resist Infect Contr 2018; 7(1): 1–10. doi: 10.1186/s13756-018-0418-x |
| 15. | Chughtai AA, Seale H, Rawlinson WD, Kunasekaran M, Macintyre CR. Selection and use of respiratory protection by healthcare workers to protect from infectious diseases in hospital settings. Ann Work Expos Health 2020; 64(4): 368–77. doi: 10.1093/annweh/wxaa020 |
| 16. | Murphy CL, McLaws M-L. Who coordinates infection control programs in Australia? Am J Infect Contr 1999; 27(3): 291–5. doi: 10.1053/ic.1999.v27.a92961 |
| 17. | Health AIo, Welfare. Health system overview. Canberra: AIHW; 2022. |
| 18. | Care ACoSaQiH. National safety and quality health service standards. 2nd ed. – version 2. Sydney: ACSQHC; 2021. |
| 19. | Gilbert GL. A brief history of 70-years’ hospital IPC in Australia. ACIPC Absttract Book 2021. Available from: https://acipcconference.com.au/events/a-brief-history-of-70-years-hospital-ipc-in-australia/ [cited 10 May 2024]. |
| 20. | Hall L, Halton K, Macbeth D, Gardner A, Mitchell B. Roles, responsibilities and scope of practice: describing the ‘state of play’for infection control professionals in Australia and New Zealand. Healthc Infect 2015; 20(1): 29–35. doi: 10.1071/HI14037 |
| 21. | McLaws M-L, Taylor P. The Hospital Infection Standardised Surveillance (HISS) programme: analysis of a two-year pilot. J Hosp Infect 2003; 53(4): 259–67. doi: 10.1053/jhin.2002.1361 |
| 22. | Morton AP, Clements AC, Doidge SR, Stackelroth J, Curtis M, Whitby M. Surveillance of healthcare-acquired infections in Queensland, Australia: data and lessons from the first 5 years. Infect Contr Hosp Epidemiol 2008; 29(8): 695–701. doi: 10.1086/589904 |
| 23. | Russo PL, Bull A, Bennett N, Boardman C, Burrell S, Motley J, et al. The establishment of a statewide surveillance program for hospital-acquired infections in large Victorian public hospitals: a report from the VICNISS Coordinating Centre. Am J Infect Contr 2006; 34(7): 430–6. doi: 10.1016/j.ajic.2005.06.013 |
| 24. | Van Gessel H, McCann RL, Peterson AM, Goggin LS. Validation of healthcare-associated Staphylococcus aureus bloodstream infection surveillance in Western Australian public hospitals. Healthc Infect 2010; 15(1): 21–5. doi: 10.1071/HI09028 |
| 25. | Arianpoor A, Zarifian A, Askari E, Akhavan-Rezayat A, Dayyani M, Rahimian A, et al. “Infection prevention and control idea challenge” contest: a fresh view on medical education and problem solving. Antimicrob Resist Infect Contr 2020; 9(1): 1–10. doi: 10.1186/s13756-020-0688-y |
| 26. | Basseal J, Bennett C, Collignon P, Currie B, Durrheim D, Leask J, et al. Key lessons from the COVID-19 public health response in Australia. Lancet Regional Health–Western Pacific 2023; 30: 100616. doi: 10.1016/j.lanwpc.2022.100616 |
| 27. | Ayton D, Tsindos T, Berkovic D. Qualitative Research: A Practical Guide for Health and Social Care Researchers and Practitioners. Australia: Council of Australian University Librarians, Open Educational Resources Collective; 2023. |
| 28. | Assariparambil AR, Nayak SG, Sugunan A, Mukhopadhyay C, Shankar R, Devi ES, et al. Structure, staffing, and factors affecting infection control nurses: hospital based exploratory survey – a study protocol. J Adv Nurs 2021; 77(2): 1062–9. doi: 10.1111/jan.14658 |
| 29. | Shaban RZ, Macbeth D, Vause N, Simon G. Documentation, composition and organisation of infection control programs and plans in Australian healthcare systems: a pilot study. Infect Dis Health. 2016;21(2):51–61. doi: 10.1016/j.idh.2016.04.002 |
| 30. | Allegranzi B, Kilpatrick C, Storr J, Kelley E, Park BJ, Donaldson L. Global infection prevention and control priorities 2018–22: a call for action. Lancet Global Health 2017; 5(12): e1178–e80. doi: 10.1016/S2214-109X(17)30427-8 |
| 31. | Zingg W, Holmes A, Dettenkofer M, Goetting T, Secci F, Clack L, et al. Hospital organisation, management, and structure for prevention of health-care-associated infection: a systematic review and expert consensus. Lancet Infect Dis. 2015; 15(2): 212–24. doi: 10.1016/S1473-3099(14)70854-0 |
| 32. | Alyahya MS, Hijazi HH, Al Qudah J, AlShyab S, AlKhalidi W. Evaluation of infection prevention and control policies, procedures, and practices: an ethnographic study. Am J Infect Contr 2018; 46(12): 1348–55. doi: 10.1016/j.ajic.2018.05.023 |
| 33. | McCauley L, Kirwan M, Matthews A. The factors contributing to missed care and non-compliance in infection prevention and control practices of nurses: a scoping review. Int J Nurs Stud Adv 2021; 3: 100039. doi: 10.1016/j.ijnsa.2021.100039 |
| 34. | McKenzie KE, Mayorga ME, Miller KE, Singh N, Arnold RC, Romero-Brufau S. Notice to comply: a systematic review of clinician compliance with guidelines surrounding acute hospital-based infection management. Am J Infect Contr 2020; 48(8): 940–7. doi: 10.1016/j.ajic.2020.02.006 |
| 35. | Cook E, Marchaim D, Kaye KS. Building a successful infection prevention program: key components, processes, and economics. Infect Dis Clin 2011; 25(1): 1–19. doi: 10.1016/j.idc.2010.11.007 |
| 36. | Brusaferro, S. Infection control in Europe. In: Walker J.T. (ed). Decontamination in Hospitals and Healthcare. Cambridge: Woodhead Publishing; 2014, 60–91. doi: 10.1533/9780857096692.1.60 |
| 37. | Gould DJ, Gallagher R, Allen D. Leadership and management for infection prevention and control: what do we have and what do we need?. J Hosp Infect. 2016; 94(2): 165–168. doi: 10.1016/j.jhin.2016.07.005 |
| 38. | Henman LJ, Corrigan R, Carrico R, Suh KN, Anderson K, Boukidjian R, et al. Identifying changes in the role of the infection preventionist through the 2014 practice analysis study conducted by the Certification Board of Infection Control and Epidemiology, Inc. Am J Infect Contr 2015; 43(7): 664–8. doi: 10.1016/j.ajic.2015.02.026 |
| 39. | Mitchell BG, MacBeth D, Halton K, Gardner A, Hall L. Resourcing hospital infection prevention and control units in Australia: a discussion paper. Infect Dis Health 2017; 22(2): 83–8. doi: 10.1016/j.idh.2017.02.001 |
| 40. | Pogorzelska M, Stone PW, Larson EL. Certification in infection control matters: impact of infection control department characteristics and policies on rates of multidrug-resistant infections. Am J Infect Contr 2012; 40(2): 96–101. doi: 10.1016/j.ajic.2011.10.002 |
| 41. | Saint S, Kowalski CP, Banaszak-Holl J, Forman J, Damschroder L, Krein SL. The importance of leadership in preventing healthcare-associated infection: results of a multisite qualitative study. Infect Contr Hosp Epidemiol 2010; 31(9): 901–7. doi: 10.1086/655459 |
Appendix 1. Survey Questions

Comparison Survey of Australia’s States and Territories HAI Programs (V1 - July 2021)
The survey will take approximately 25 minutes to complete. Completion is voluntary, individuals will not be identified. Characteristics of State and National Healthcare associated Infection programs - a comparison study of Infection Prevention and Control (IPA() elements in each states program
* Required
Name of State or Territory
○ NSW
○ Queensland
○ South Australia
○ Tasmania
○ Victoria
○ Western Australia
○ Australian Capital Territory
○ Northern Territory
○ ACSQHC-HAI Jurisdictional Steering Committee
Years of Experience in Infection Prevention and Control?

Years in State/Health service Role

How many people are in your team ? (BAU)

How Many in Your Team in response to COVID?

Name Of Program

Do you have a state-wide IPAC program?
○ Yes
○ No
○ Other
If you answered No to question 7 would you prefer one?
○ Yes
○ Other
What would you like to see in your state wide program ? e,g, expectations

Is the focus of your statewide Infection Prevention and Control program or Health Care Associated Infection program focused on
○ HAI
○ IPAC
○ Focus on both HAI and IPAC
○ Focus on IPAC increase only since COVID-19
○ Other
Indicate your routine state/national IPC/HAI program content (Tick all that applies)
□ IPAC principles
□ HAI
□ Transmission Based Precautions
□ Environmental Cleaning
□ Reprocessing reusable Medical devices
□ Multi drug resistant Organisms and emerging pathogens
□ High Consequence Infectious Diseases
□ Device Related infections and resources or tool kits
□ Surveillance (SSI, SAB CDI)
□ Governance, quality and risk
□ Procurement, redevelopment and new construction
□ Incident/Outbreak Management
□ Other
The health system and the clinicians you serve understand the statewide HAI program also leads IPAC
○ Extremely Agree
○ Strongly Agree
○ Agree
○ Neither agree or disagree
○ disagree
○ Strongly disagree
○ Extremely disagree
Is the state HAI program consistent with The Australian Commission on Safety and Quality in HealthCare Standard in regard to HAI/IPC
○ Definitely
○ Somewhat
○ Not at all
Where does your HAI/IPC program sit in THE organisational chart AND IS Governance CLEAR
□ Patient Safety
□ Health protection/Public Health
□ Communicable Diseases
□ Other
□ Yes governance is clear
□ No governance is not clear
How many trained infection prevention and control staff are in the state IPC program/team (Pre COVID)
Please indicate numbers.
*
Number of Infection Prevention and Control Practitioners in statewide program (ICPs):
□ 1 Full time ICP staff
□ 2 Full Time ICP Staff
□ 3 Full Time ICP Staff
□ > 3 Full Time ICP Staff (record Number in Comments)
□ 1 Part time ICP staff
□ 2 Part time ICP staff
□ 3 Part time ICP staff
□ >3 Part time ICP staff (record Number in Comments)
□ Nil ICPs
□ Staff Credentialed as ICPs
□ CICP-E (Expert Credential)
□ CICP-A (Advanced Credential)
□ CICP-P (Primary Credential)
□ Other (provide detail Q16)
Comment for Question 15 including additional numbers*

Is your statewide program led by an ICP?
○ Yes
○ No
If your answer to 017 is No please write down classification of your statewide program lead

Indicate the professional groups who are employed at the statewide/territory level as part of the program to implement the state/territory program
□ IPC Practitioner
□ Infectious disease or microbiologist physician/doctor
□ Non specialist medical officer
□ Public Health doctor
□ Environmental health officer
□ Research officer/assistant
□ Data Manager
□ Information technology expert
□ Project Officer
□ Project Support/Administrative support
□ Other
Doyou feels the term and focus on HAI diminished the overarching specialty of Infection Prevention And Control as understood by clinicians
○ Extremely Agree
○ Strongly Agree
○ Agree
○ Neither Agree or Disagree
○ Strongly Disagree
○ Extremely Disagree
Comment for Q20 Below

During COVID-19 the IPAC response was the responsibility of the same program responsible for IPAC and COVID?
○ Definitely
○ Somewhat
○ Not at all
If answer to question 22 is not at all, who (agency/organisation) became responsible for IPAC during COVID-19?

The structure for your state HAI/IPAC PROGRAM(S) ENABLED A well prepared RESPONSE TO COVID-19 pandemic?
○ Extremely Agree
○ Strongly Agree
○ Agree
○ Neither Agree or Disagree
○ Disagree
○ Strongly disagree
○ Extremely disagree
Comment for Q24

Please provide any additional comment or suggestions here.

 Partial component – some elements are included but not considered a complete suite of strategies; for example NSW has a statewide mandatory clinical indicator requirement but no statewide surveillance system or database.
Partial component – some elements are included but not considered a complete suite of strategies; for example NSW has a statewide mandatory clinical indicator requirement but no statewide surveillance system or database.