REVIEW ARTICLE
The physical effects of wearing personal protective equipment: a scoping review
Lyvonne N. Tume1,2*, Davide Ungari2, Fariba Bannerman3, Sean Cuddihy2, Claire Gnanalingham4 and Hayley Phillips4
1School of Health & Society, University of Salford, Manchester, UK; 2Paediatric Intensive Care Unit (PICU), Alder Hey Children’s Hospital, Liverpool, UK; 3Alder Hey Library, Alder Hey Children’s Hospital, East Prescot Road, Liverpool, L12 2AP, UK; 4Alder Hey Children’s Hospital, Liverpool, UK
Abstract
Background: The COVID-19 pandemic has required healthcare workers to wear personal protective equipment (PPE), and although there is increasing awareness of the physical effects of wearing PPE, the literature has yet to be synthesised around this topic.
Methods: A scoping review was conducted to synthesise existing literature on the physical effects of wearing PPE and identify gaps in the literature. A comprehensive search strategy was undertaken using five databases from 1995 to July 2020.
Results: A total of 375 relevant articles were identified and screened. Twenty-three studies were included in this review. Studies were conducted across 10 countries, spanning 16 years from 2004 to 2020. Half (13/23) were randomised controlled trials or quasi-experimental studies, five surveys, two qualitative studies, two observational or case series and one Delphi study. Most (82%, 19/23) studies involved the N95 mask (either valved or unvalved). None specifically studied the filtering facepiece 3 mask. The main physical effects relate to skin irritation, pressure ulcers, fatigue, increased breathing resistance, increased carbon dioxide rebreathing, heat around the face, impaired communication and wearer reported discomfort. Few studies examined the impact of prolonged wear (akin to real life practice) on the physical effects, and different types of PPE had different effects.
Conclusions: The physical effects of wearing PPE are not insignificant. Few studies examined the physiological impact of wearing respiratory protective devices for prolonged periods whilst conducting usual nursing activity. No ideal respirators for healthcare workers exist, and the development of more ergonomic designs of PPE is required.
Keywords: healthcare workers; personal protective equipment; physical effects; physiological effects; review
Citation: Int J Infect Control 2022, 18: 22415 – http://dx.doi.org/10.3396/ijic.v18.22415
Copyright: © 2022 Lyvonne N. Tume et al. This is an Open Access article distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for any purpose, even commercially, provided the original work is properly cited and states its license.
Received: 10 January 2022; Accepted: 28 March 2022; Published: 3 June 2022
Competing interests and funding: The authors declare that there are no conflicts of interest to declare. This work is not funded.
*Lyvonne N. Tume, School health & Society, University of Salford, Manchester Uk, M6 6PU, UK. Email: l.n.tume@salford.ac.uk
To access the supplementary material, please visit the article landing page
The COVID-19 pandemic has brought the issue of wearing appropriate (to risk level), effective personal protective equipment (PPE) to the forefront for healthcare workers (healthcare professionals, HCPs). Important issues for staff at high risk (such as those in critical care units) are not only both the availability and correct fit of the PPE but also the physical impact of wearing PPE for prolonged periods when undertaking active clinical work. Previous systematic reviews have focused on adherence to wearing PPE by HCPs (1), the effectiveness of respirators and other measures in reducing the risk of infection in HCPs or others (2–4), comparing effectiveness between surgical masks and N95 masks in respiratory infection (5), but no paper has mapped the current evidence around the physical and physiological impacts of wearing PPE (for prolonged periods) on HCPs. The objective of this scoping review is, therefore, to map current evidence around the physical and physiological adverse effects and staff experience of wearing PPE for respiratory-transmitted infections. This will inform future decision-making and highlight gaps in the evidence base to inform future research.
Methods
This scoping review was undertaken using the five-stage scoping review method described by Arksey and O’Malley (6). Stage 1: identifying the research question; Stage 2: identifying relevant studies; Stage 3: study selection; Stage 4: charting the data and Stage 5: collating, summarising and reporting the results. In this study, PPE was defined as wearing any component of respiratory protective devices (RPDs), eye protection, gown and gloves, for protection against respiratory-transmitted infections. This study has conformed to the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) reporting checklist for scoping reviews (7) and is registered in OSF.HOME as a scoping review.
Stage 1: Identifying the research question
Our questions were developed in response to both a clinical and research need and are as follows: In HCPs (human participants) wearing PPE for respiratory-transmitted infections:
- What are the physiological and physical effects?
- What are the adverse effects of wearing PPE?
- How do staff experience the physical effects of working in PPE?
Stage 2: Identifying relevant studies
We developed our search strategy in consultation with a medical information specialist (FB) who searched the following bibliographic electronic databases: MEDLINE, EMBASE, The Cochrane Library and CINAHL, using the Health Databases Advanced Search (HDAS) platform between 10 June and 8 July 2020 using the search terms listed in Table 1. We also searched the PROSPERO systematic review database and Google Scholar to capture any items not previously identified. We screened reference lists of included studies and relevant reviews. The search strategies for each database can be found in Supplementary File 1.
We included papers from 1995 onwards (25 years) to include other respiratory pandemics: severe acute respiratory syndrome (SARS) (2003), influenza A H1N1 (2009) and other influenzas, in addition to COVID-19. Only papers published in English were included, and we included both quantitative and qualitative research studies if the physical effects of wearing one or more components of PPE (defined previously) were studied or reported, if they were conducted in humans or HCPs or surveys where they examined HCPs perceived physical effects. Grey literature was searched, and any previously unidentified references were identified, but these are not included in the review. We excluded papers that examined HCPs ability to perform certain tasks (e.g. resuscitation) wearing PPE, those relating to adherence to PPE and contamination during donning and doffing, entirely laboratory or simulation based studies where the physical impact on humans was not studied, and studies specifically in pregnant women as this has been previously reported. This scoping review is also not looking at mask/PPE effectiveness, so papers examining this were excluded. General discussion papers, opinion pieces and non-English papers were also excluded.
Stage 3: Article selection
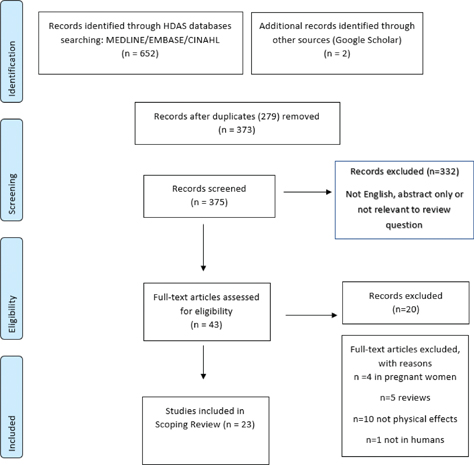
Stage 3 involved the clinical members of the study team (LT, DU, SC, CG and HP), screening all retrieved abstracts for potential inclusion, by applying the inclusion and exclusion criteria above. All abstracts were screened by two reviewers, and any discrepancies or ambiguity resolved by discussion with LT. If the relevance of a study was unclear from the abstract, then the full article was obtained (Fig. 1).
Stage 4: charting and extracting the data
The next stage involved data extraction and ‘charting’ key items of information obtained from the primary research studies. Data extraction templates were created: qualitative papers (key themes identified) and quantitative papers (numerical data extraction). Data were extracted into an evidence table (developed a priori), and this was checked for accuracy by the lead author (LT).
Stage 5: collating, summarising, and reporting the results
First, tables and chart mapping have been produced for the types of PPE studied, the physical effects and the time spent in PPE. Second, the literature has been organised thematically according to different physical effects reported with PPE.
Results
Three hundred and seventy-five research papers were identified through the searches (after duplicates removed) and screened. Six pieces of grey literature were located (these were national, professional society or company guidance and are not primary evidence included in the review), full text was obtained for 43 papers, and 23 research papers met the inclusion criteria and are included in the review (Fig. 1). Studies were conducted across 10 countries, spanning 16 years from 2004 to 2020. Half (13/23) were randomised controlled trials or quasi-experimental studies, five surveys, two qualitative studies, two observational or case series and one Delphi study (Table 2).
Different types of PPE were studied (Fig. 2), most commonly RPDs, and of these, 82% (19/23) were N95 masks (either valved or unvalved).
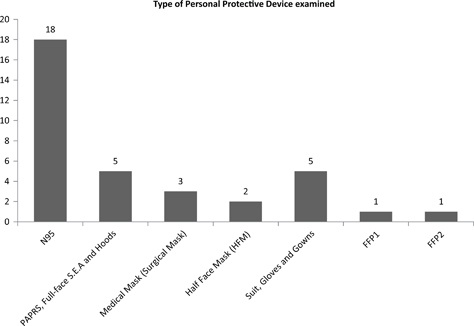
Fig. 2. Types of personal protective equipment examined in the number of studies. S.E.A. is a modified full face mask brand. Y axis represents the number of studies.
Figures 3 and 4 summarise the main physical effects common to PPE. None of them specifically studied the model most used within Europe and the UK, the filtering facepiece (FFP) 3 mask, although other RPDs (like the N95) may produce similar effects.
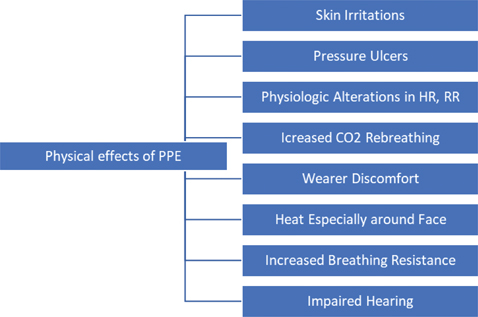
Fig. 3. Map of scoping review physical effects.
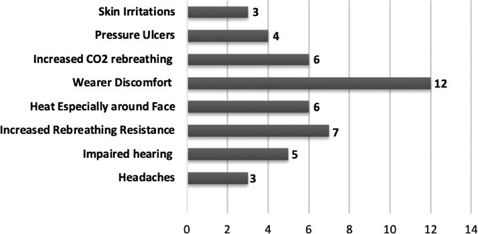
Fig. 4. The physical effects of personal protective equipment reported by study. X axis represents number of studies in which physical effects were cited.
The results of this review are categorised into six main themes:
- HCP reported physical effects of wearing PPE
- The respiratory effects wearing different masks/respirators
- Other effects of different mask/respirator
- The physical effects of wearing PPE on the skin
- Staff preferences of PPE type
- The impact of time and duration on the physical effects of wearing PPE
Healthcare professionals reported physical effects of wearing PPE
Eight of the studies (8–15) examined the reported physical effects of wearing PPE in HCPs: five survey designs including Delphi studies (9–11, 13, 15), one case series (8), one mixed method study (12) and one qualitative study (14). These studies were conducted in Singapore, Malaysia, the United States, China, Australia, Israel, Portugal and Iran from 2006 to 2020. Two of these focused specifically on skin effects, and these are discussed under that heading, with one study focusing specifically on headaches. Lim et al. (11) surveyed 212 HCPs about headaches when wearing the N95 mask. Thirty-seven percent reported headaches when wearing the N95, and over half of these (55%) had worn the mask continuously for >4 h. Staff who suffered from preexisting headaches suffered this symptom significantly more (P = 0.01). In a study (12) performed in Australia during the H1N1 pandemic, staff reported how difficult and uncomfortable wearing full PPE was and the impaired communication associated with it. A Delphi study (13) aimed to identify physical effects that acted as barriers to using the N95 mask in HCPs in Iran. They found six factors (four of these physical effects are as follows: heat around the face, difficulty breathing, pressure on the nose and trouble in communication) as the most important barriers for staff using N95 respirators. Finally, a 10-item self-report survey (15) examined the key human factors: physical and ergonomic, perceptual and cognitive, which influence the use of level 1 PPE worn during the COVID-19 pandemic. In total, 722 HCPs in Israel and 301 from Portugal were surveyed (a mixture of males/females and nurses, physicians and allied health personnel). All respondents had worn level 1 PPE for at least a few hours daily to several hours weekly. They found high levels of perceived difficulty, with medians of 4/5 for items related to discomfort, hearing, and seeing and doffing. A subsequent analysis showed an association between PPE discomfort with impaired situational awareness (P ≤ 0.01), with this association mediated by difficulties in hearing and understanding speech, reflecting difficulties in communication. Radonovich et al. (16) studied factors that resulted in mask intolerance by 27 HCPs. Heat and facial discomfort, impaired communication and other somatic effects (dizziness, nausea and itching) were the main factors contributing to this ‘intolerance’ of RPDs that necessitated removal of the device. They noted that women were significantly more likely to report intolerance than men.
The respiratory effects of wearing different masks/respirators
Twelve of 22 studies (13, 16–26) analysed the respiratory effects of wearing different respirators. These studies were conducted in Singapore (n = 2), Hong Kong (n = 1), the United States (n = 6), Australia (n = 1), Turkey (n = 1) and Iran (n = 1) from 2004 to 2020. The respiratory effects can be broadly divided in three themes: an increase in carbon dioxide (CO2) rebreathing, an increase in breathing resistance and the effect on arterial oxygen saturations (SpO2).
Smith et al. (17), in an exercise laboratory study, examined the physical consequences of speech and work rates and found that incremental CO2 rebreathing occurs in RPDs. A quasi-experimental study (22) in healthy HCPs found that FFP respirators broadly did not have any significant physiological impact during 1 h of utilisation. However, the FFP respirator’s dead-space, carbon dioxide and oxygen levels varied from the recommended working environmental standards, and elevated CO2 levels were possible. In addition, the FFP’s effect on CO2 clearance was not enhanced by having an exhalation valve. In contrast, Randovich et al. (16) in a crossover trial of 27 HCPs found that wearing a N95 mask without an exhalation valve was associated with more intolerance than a similar model with a valve. Özdemir et al. (23) also examined end tidal CO2 (EtCO2) values of participants wearing PPE over time. They found that a statistically significant difference from that at baseline (P ˂ 0.003) and after the 10th minute of wearing PPE CO2 levels significantly exceeded baseline levels (P = 0.005). The use of an FFP2 respirator with a surgical mask cover considerably worsened the EtCO2 and fractional concentration of inspired CO2 (FiCO2) values in participants. However, both Rebmann (24), in a randomised crossover trial of 10 nurses wearing N95 masks and Powell (25), in a prospective observational study of 12 adults, noted that although CO2 levels were higher than at baseline, the changes were unlikely to be clinically significant.
The increase in breathing resistance is amongst the most important reported problems in HCPs wearing N95 respirators (13). Most of the studies report wearers perceived difficulty in breathing in RPDs, despite little evidence of any clinically significant physiological effects (24). Lee et al. (18) found a rise in nasal resistance after the removal of the N95 and surgical masks after 3 h of use, potentially due to nasal physiological changes. However, this study is limited by few (n = 14) participants and the inadequate duration of time monitored after mask removal to allow nasal resistance to return to baseline. Li et al. (19) in a quasi-experimental study of 10 participants found a substantial difference between the N95 and surgical masks, in addition to an alteration of the physiological parameters and wearer discomfort. Respiratory resistance was significantly (P ≤ 0.01) higher in the N95 masks compared to the surgical mask, and subjective perception of breathing difficulty and discomfort also increased significantly with increasing thermal stress. Bansal et al. (20) compared the physiological impact of two RPDs in simulated work conditions (a dual cartridge half face mask respirator [HFM] and the N95 respirator) in 56 participants. They found that tidal volume, minute ventilation, breathing frequency and heart rate were all significantly higher in higher workload tasks. Despite this, they suggest that for most individuals, including those with mild respiratory distress, both types of RPD could be tolerated physiologically.
Three studies specifically examined the changes in SpO2 in relation to the use of PPE. Two (21, 22) found no statistical difference observed between pre, during or post PPE use with regards to SpO2, compared to the other physiologic parameters. They also found no significant differences between the type of RPD worn. Powell et al. (25) studied 12 healthy adults in a prospective observational study in a temperate environment during low–moderate work over 1 h, wearing a loose-fitting or tight-fitting powered air purifying respirator (PAPR). They found no impact on SpO2 (or other physiologic parameters), or perceptions of breathing effort, respiration discomfort, associated ratings of perceived effort, other than that of wearing a N95 mask.
Other non-respiratory physical effects of wearing respirators or masks
Several other physical effects of wearing masks or RPD are apparent in these studies—the most common being facial heat, pain and pressure over the nose/ears, but headaches, light-headedness, pressure and skin irritations along with communication difficulties are also reported. Honarbakhsh et al. (13) in their Delphi survey of clinicians and infection control experts concluded that heat around the face and trouble in communication were the two top physical factors. Likewise, others (27) also noted facial heat, pain and pressure as other non-respiratory reported effects. Lam et al. (8) specifically studied headaches in HCPs wearing PPE and found these were worse in HCPs with existing headaches, and the likelihood of headache increased as time in PPE increased to near and beyond 4 h. Two studies specifically focused on skin irritation and pressure ulcers (8, 9), and these are discussed in the next theme. Importantly, in healthcare settings, communication difficulties both with hearing and speech are consistently reported in HCPs wearing PPE (12, 13, 15, 24). Parush et al. (15), in a large survey with over 1,000 responses across two countries, noted this and identified this impaired ability to communicate/understand significantly impaired situational awareness, which is critical for safety in a healthcare environment. Radonovich et al. (16) in an unblinded crossover trial of 27 HCPs found that heat and facial discomfort, impaired communication and other somatic effects (dizziness, nausea and itching) were the main factors contributing to ‘intolerance’ of RPDs that necessitated removal of the device. They noted women were significantly more likely to report intolerance than men, and wearing a N95 mask without an exhalation valve was associated with more intolerance than a similar model with a valve.
The physical effects of wearing PPE on the skin
Skin lesions and irritation were commonly reported in individuals wearing PPE. A case series (8) specifically reported pressure ulcers on the dorsum of the nose related to wearing an N95 mask in five HCPs, ranging from grade 1 to grade 3. In a survey of 322 HCPs in Singapore (9), other reported skin problems were acne (60%), facial itch (51%) and rashes (36%) whilst wearing the N95 mask. HCPs reporting acne were significantly younger than those who without. Prolonged wear of the N95 mask appeared to worsen the effect of these. A further survey of 65 HCPs in China (10) also found skin irritation, and in addition to those symptoms noted above, they found dry skin (26%), scarring of the nasal bridge (69%), wheals (11%), indentation and ear pain (11%) and desquamation (10%) associated with wearing the N95 mask. They also noted other skin effects related to the wearing of disposable gloves, with 64 (21.4%) of the 299 staff who used gloves regularly reporting adverse skin reactions, including dry skin (73.4%), itch (56.3%), rash (37.5%) and wheals (6.3%). Staff who reported dry skin and itching were younger compared with staff who did not. Hu et al. (10) also found staff reported skin issues related to wearing gloves: dry skin (55.8%), itching (31.2%), rashes (23.0%), chapped skin (21.3%), wheals (8.2%), skin soaked with sweat (4.9%) and edema (1.6%). Some of these effects are also inherently linked with frequent handwashing associated with managing infected patients. Few skin effects were associated with the wearing of disposable gowns. Two of the survey studies reported these: Foo et al. (9) found that only 1.6% of the staff who wore gowns regularly reported adverse skin reactions, whereas Hu et al. (10) found a higher rate of adverse skin reactions from using protective clothing: dry skin (22 of 65, 36.1%), itching (21, 34.4%), rashes (7, 11.5%) and wheals (2, 3.3%).
Staff preferences of PPE type
Undoubtedly, discomfort is the most reported physical effect perceived by HCPs wearing PPE. However, discomfort varies with the type of PPE worn and undoubtedly with the individual. This inevitably leads HCPs to prefer one type of PPE over another. Hines et al. (28) surveyed 2,252 HCPs on user acceptance of reusable respirators in health care (24% wearing elastomeric half-face respirator [EHFR], 53% wearing N95 respirators and 23% wearing PAPRs). In relation to perceived comfort, N95 users rated their respirators significantly more favourably than did either EHFR (P < 0.001) or PAPR users (P < 0.001). Regarding communication, N95 users again rated their respirators more favourably in comparison to EHFR (P < 0.001) or PAPR users (P < 0.001). Despite these preferences, when participants were asked about providing protection for them, EHFR users rated their respirators more favourably. Both EHFR (P < 0.001) and PAPR (P = 0.012) users rated their masks significantly more favourably than N95 users, based on their fit test. This contrasts with N95 users (P = 0.003), who would have needed a similar fit test, compared to PAPR users (P = 0.005), who still require training despite not having to undergo fit test.
The impact of time and duration on the physical effects of wearing PPE
Nineteen studies reported the duration of time participants were studied in PPE (8–12, 16, 27, 29, 30) (Fig. 5). The maximum time studied in PPE ranged from 5 to 720 min, and in the few studies, this ranged from 5 to 199 min, reporting the minimum time (20, 24, 25, 29). All studies that examined the physical effects over time found effects worsened with increasing time. Rebmann et al. (24) found that perceived exertion, shortness of breath, headache and light-headedness all increased over time with 22% of early PPE removals due to discomfort. Zhu et al. (26) also noted that mean comfort reduced as length of time wearing the N95 mask increased. Corley et al. (12) found staff (in practice) were expected to wear full PPE for 12 h shifts with a 1–1.5-h break (reflecting real life practice), and staff reported significant difficulties with this as time increased. Foo (9) and Shenal (27) also found staff perceived discomfort over time, with Shenal finding facial heat, pain and pressure the worse effects that increased over time (in an 8-h period). Loibner et al. (29) studied the effect of wearing two types of full PPE suits; both were uncomfortable for staff, and the effects of this discomfort worsened as the time in the suit increased. Radonovich (16) found that 59% of HCPs discontinued wearing the respirator ensembles before 8 h reporting a variety of reasons for this intolerance, including communication interference, along with physical effects.
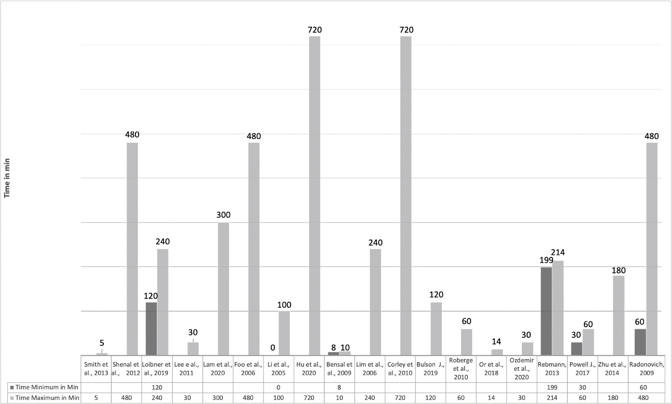
Fig. 5. Time spent in PPE as reported by study.
Discussion
We used a systematic methodology and searched a range of databases to capture the full range of existing studies on the physical effects of PPE in HCPs. This review has achieved the study objectives. First, this scoping review has identified the most common physical and physiological effects and adverse effects of wearing PPE. These effects (summarised in Fig. 3) are most commonly respiratory effects, pressure ulcers, other skin irritations, heat, impaired communication and general wearer discomfort. Staff experience wearing PPE is generally negative, although use is recognised as essential. Impaired communication and wearer discomfort, which worsen over time, have been shown.
This review highlights the gaps in research, especially specifically around the FFP 3 mask (used most within the United Kingdom), and the differences between this and other RPD types such as the N95 and FFP2. Furthermore, as RPDs vary in design and level of protection, one RPD type will not provide the same level of comfort to all HCPs. Historically, PPE and RPDs were designed for men in industrial situations (31), yet many healthcare workers (especially nurses) are female and from multiple ethnic backgrounds in the United Kingdom; this has implications for the ‘fit’ and comfort of RPDs, and this has not been adequately researched. Future studies need to explore this. Improving the acceptability and usability of wearing PPE for HCPs, including ease of communication and physical comfort, was identified as a research priority in 2010 by a large US report funded by the US Institute of Medicine, yet this remains a significant gap in research (32).
Currently no ‘ideal’ RPDs for HCPs exist, and we know that a ‘one size fits all’ approach does not work (33). More research is urgently required to develop a more individualised approach to RPD fitting and wearing, to maximise comfort for staff. Some of the studies compared both valved and non-valved RPDs, not showing any significant different in respiratory effects. Valved RPDs are designed to make expiration easier, and thus more comfortable to wear, with less moisture build up inside the mask (34). The downside to this is the failure to filter the wearers exhalation, providing only one-way protection (for the wearer) and potentially placing others at risk (34). During COVID-19, with reported widescale asymptomatic infections (some of these amongst HCPs) and many patients in hospital settings, especially in intensive care units, not required or able to wear masks, this potentially puts them at risk (35).
Gaps in the literature
There are clear gaps in the evidence identified from this scoping review. No UK studies exist, and no studies have specifically examined the impact of FFP3 masks (worn extensively in the UK and Europe); although likely to be similar to the N95, this is not known. Furthermore, there is limited evidence on the physiological impact of wearing PPE (in particular RPDs) for more than 2 h whilst conducting moderate nursing tasks in standard hospital temperatures, recommended to be 18°C (36), and comparing different ethnic groups with different physical facial features.
Limitations
There are several limitations to this scoping review, although it was based on a comprehensive review of the literature, with expertise from an information specialist. It is possible that some relevant studies were missed, as we only included studies published in English. We also excluded studies that specifically examined HCPs’ ability to perform, non-human laboratory or simulation-based studies, and those studies specifically of pregnant women as this has been previously reported (37). A further limitation of our methods is that papers are not critically appraised in depth and the evidence level graded; however, what we have done is map the literature on this topic and identified gaps for further research as well as the clinical implications.
Clinical implications of the scoping review
The physical effects of wearing PPE (even RPDs alone) are not insignificant, and these effects are magnified over time and in warmer environments. Managers must be highly cognisant of these effects and ensure HCPs have adequate frequent breaks from PPE and, where possible, the environmental temperature modified to improve comfort. This requires both a review of staffing and working practices to facilitate. Adequate occupational health input is also important to prevent, reduce (where possible) or treat these physical effects in HCPs. History suggests that this pandemic will not be the last, thus further research and development of newer more ergonomic PPE is essential.
Conclusions
Currently, no ‘ideal’ PPE exists for HCPs, with numerous physical effects reported and quantified. Working effectively in PPE continues to be challenging, since it is necessary for clinical staff to wear PPE for prolonged periods. Having knowledge of these physical effects directs future designers of PPE to develop more ergonomic designs and researchers to gaps in our knowledge, especially around the impact of FFP3 masks worn in the United Kingdom. This knowledge also directs managers to reconsider the work pattern and staffing levels required for staff working in PPE to ensure more frequent breaks can be undertaken to ensure both worker safety and effective and safe care delivery.
Ethical considerations
Ethics approval was not required for this study.
References
- Houghton C, Meskell P, Delaney H, Smalle M, Glenton C, Booth A, et al. Barriers and facilitators to healthcare workers’ adherence with infection prevention and control (IPC) guidelines for respiratory infectious diseases: a rapid qualitative evidence synthesis. Cochrane Database Syst Rev 2020; 4(4): CD013582. doi: 10.1002/14651858.CD013582
- Cowling BJ, Zhou Y, Ip DK, Leung GM, Aiello AE. Face masks to prevent transmission of influenza virus: a systematic review. Epidemiol Infect 2010 Apr; 138(4): 449–56. doi: 10.1017/S0950268809991658
- Chou FR, Dana T, Jungbauer R, Weeks C, McDonagh MS. Masks for prevention of respiratory virus infections, including SARS-CoV-2, in health care and community settings: a living rapid review. Ann Intern Med 2020; 173(7): 542–55. doi: 10.7326/M20-3213
- bin-Reza F, Lopez Chavarrias V, Nicoll A, Chamberland ME. The use of masks and respirators to prevent transmission of influenza: a systematic review of the scientific evidence: masks and respirators to prevent influenza. Influenza Other Respir Viruses 2012; 6(4): 257–67. doi: 10.1111/j.1750-2659.2011.00307.x
- Smith JD, MacDougall CC, Johnstone J, Copes RA, Schwartz B, Garber GE. Effectiveness of N95 respirators versus surgical masks in protecting health care workers from acute respiratory infection: a systematic review and meta-analysis. Can Med Assoc J 2016; 188(8): 567–74. doi: 10.1503/cmaj.150835
- Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol 2005; 8(1): 19–32. doi: 10.1080/1364557032000119616
- Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med 2018; 169(7): 467–73. doi: 10.7326/M18-0850
- Lam U, Md. Mydin Siddik NSF, Mohd Yussof SJ, Ibrahim S. N95 respirator associated pressure ulcer amongst COVID -19 health care workers. Int Wound J 2020; 17(5): 1525–7. doi: 10.1111/iwj.13398
- Foo C, Goon A, Leow Y, Goh C. Adverse skin reactions to personal protective equipment against severe acute respiratory syndrome- a descriptive study in Singapore. Contact Dermatitis 2006; 55(5): 291–4. doi: 10.1111/j.1600-0536.2006.00953.x
- Hu K, Fan J, Li X, Gou X, Li X, Zhou X. The adverse skin reactions of health care workers using personal protective equipment for COVID-19. Medicine 2020; 99(24), e20603. doi: 10.1097/MD.0000000000020603
- Lim E, Seet R, Lee K, Wilder-Smith EPV, Chuah BYS, Ong BKC. Headaches and the N95 facemask amongst healthcare providers. Acta Neurol Scand 2006; 113(3): 199–202. doi: 10.1111/j.1600-0404.2005.00560.x
- Corley A, Hammond NE, Fraser JF. The experiences of health care workers employed in an Australian intensive care unit during the H1N1 Influenza pandemic of 2009: a phenomenological study. Int J Nurs Stud 2010; 47(5): 577–85. doi: 10.1016/j.ijnurstu.2009.11.015
- Honarbakhsh M, Jahangiri M, Farhadi P. Effective factors on not using the N95 respirators among health care workers: application of fuzzy delphi and fuzzy analytic hierarchy process (FAHP). J Healthc Risk Manag 2017; 37(2): 36–46. doi: 10.1002/jhrm.21286
- Locatelli SM, LaVela SL, Gosch M. Health care workers’ reported discomfort while wearing filtering face-piece respirators. Workplace Health Saf 2014; 62(9): 362–8. doi: 10.3928/21650799-20140804-03
- Parush A, Wacht O, Gomes R, Frenkel A Human factor considerations in using personal protective equipment in the COVID-19 pandemic context: binational survey study. J Med Internet Res 2020; 22(6):e19947. doi: 10.2196/19947
- Radonovich LJ Jr, Cheng J, Shenal BV, Hodgson M, Bender BS. Respirator tolerance in health care workers. J Am Med Assoc 2009 Jan 7; 301(1): 36–8. doi: 10.1001/jama.2008.894
- Smith CL, Whitelaw JL, Davies B. Carbon dioxide rebreathing in respiratory protective devices: influence of speech and work rate in full-face masks. Ergonomics 2013; 56(5): 781–90. doi: 10.1080/00140139.2013.777128
- Lee HP, Wang de Y. Objective assessment of increase in breathing resistance of N95 respirators on human subjects. Ann Occup Hyg 2011; Oct; 55(8): 917–21. doi: 10.1093/annhyg/mer065
- Li Y, Tokura H, Guo YP, Wong ASW, Wong T, Chung J, et al. Effects of wearing N95 and surgical facemasks on heart rate, thermal stress and subjective sensations. Int Archiv Occup Environ Health 2005; 78(6): 501–9. doi: 10.1007/s00420-004-0584-4
- Bansal S, Harber P, Yun D, Liu D, Liu Y, Wu S, et al. Respirator physiological effects under simulated work conditions. J Occup Environ Hyg 2009; 6(4): 221–7. doi: 10.1080/15459620902729218
- Bulson D, Shawl K. Understanding the physiological effects of wearing enhanced personal protective equipment while providing patient care. J Emerg Manag 2019; 17(6): 517–21. doi: 10.5055/jem.2019.0444
- Roberge RJ, Coca A, Williams WJ, Powell JB, Palmiero AJ. Physiological impact of the N95 filtering facepiece respirator on healthcare workers. Respir Care 2010; 55(5): 569–77.
- Özdemir L, Azizoğlu M, Yapıcı D. Respirators used by healthcare workers due to the COVID-19 outbreak increase end-tidal carbon dioxide and fractional inspired carbon dioxide pressure. J Clin Anesth 2020; 66: 109901. doi: 10.1016/j.jclinane.2020.109901
- Rebmann T, Carrico R, Wang J. Physiologic and other effects and compliance with long-term respirator use among medical intensive care unit nurses. Am J Infect Control 2013; 41(12): 1218–23. doi: 10.1016/j.ajic.2013.02.017
- Powell JB, Kim JH, Roberge RJ. Powered air-purifying respirator use in healthcare: effects on thermal sensations and comfort. J Occup Environ Hyg 2017; 14(12): 947–54. doi: 10.1080/15459624.2017.1358817
- Zhu JH, Lee SJ, Wang DY, ÿLee H. Effects of long-duration wearing of N95 respirator and surgical facemask: a pilot study. J Lung Pulm Respir Res 2014; 1(4): 97–100. doi: 10.15406/jlprr.2014.01.00021
- Shenal BV, Radonovich LJ, Cheng J, Hodgson M, Bender BS. Discomfort and exertion associated with prolonged wear of respiratory protection in a health care setting. J Occup Environ Hyg 2012; 9(1): 59–64. doi: 10.1080/15459624.2012.635133
- Hines SE, Brown C, Oliver M, Gucer P, Frisch M, Hogan R, et al. User acceptance of reusable respirators in health care. Am J Infect Control 2019; 47(6): 648–55. doi: 10.1016/j.ajic.2018.11.021
- Loibner M, Hagauer S, Schwantzer G, Berghold A, Zatloukal K. Limiting factors for wearing personal protective equipment (PPE) in a health care environment evaluated in a randomised study. PLoS One 2019; 14(1): e0210775. doi: 10.1371/journal.pone.0210775
- Or P, Chung J, Wong T. A study of environmental factors affecting nurses’ comfort and protection in wearing N95 respirators during bedside procedures. J Clin Nurs 2018; 27: e1477–84. doi: 10.1111/jocn.14268
- Gharni R. Is PPE working for women? Occup Health 2017; 13(6): 32–5.
- Larson EL, Liverman CT. Editors. Institute of Medicine (US) Committee on Personal Protective Equipment for Healthcare Personnel to Prevent Transmission of Pandemic Influenza and Other Viral Respiratory Infections: Current Research Issues. Preventing transmission of pandemic influenza and other viral respiratory diseases: personal protective equipment for healthcare personnel: update 2010. Washington, DC: National Academies Press (US). Available from: https://www.ncbi.nlm.nih.gov/books/NBK209584/ [cited 3 October 2020].
- Fidler H. PPE: ‘One size fits all’ design is a fallacy that’s putting female health staff at risk. RCNi; 2020 May 4. Available from: https://rcni-com.salford.idm.oclc.org/nursing-standard/opinion/comment/ppe-one-size-fits-all-design-a-fallacy-thats-putting-female-health-staff-risk-160536 [cited 3 October 2020].
- Chang JC, Johnson JS, Olmsted RN. Demystifying theoretical concerns involving respirators with exhalation valves during COVID-19 pandemic. Am J Infect Control 2020; 48(12): 1564–5. doi: 10.1016/j.ajic.2020.08.031
- Gao Z, Yinghui Xu Y, Sun C, Wang X, Guo Y, Qiu S, et al. A systematic review of asymptomatic infections with COVID-19. J Microbiol Immunol Infect 2021; 54(1): 12–6. doi: 10.1016/j.jmii.2020.05.001
- Unison. Health and safety information sheet: temperatures at work. 2014. Available from: https://www.unison.org.uk/content/uploads/2013/06/Briefings-and-CircularsTemperature-at-Work-Information-Health-and-Safety-Information-Sheet2.pdf [cited 3 October 2020].
- Roeckner JT, Krstić N, Sipe BH, Običan SG. N95 filtering facepiece respirator use during pregnancy: a systematic review. Am J Perinatol 2020; 37(10): 995–1001. doi: 10.1055/s-0040-1712475