ORIGINAL ARTICLE
Sliding doors: how does their opening affect particulate matter levels in operating theatres?
Alessandro Della Camera1, Gabriele Cevenini2, Nicola Nante1,3, Maria Francesca De Marco4 and Gabriele Messina1,3*
1Post Graduate School of Public Health, Department of Molecular and Developmental Medicine, University of Siena, Siena, Italy; 2Department of Medical Biotechnologies, University of Siena, Siena, Italy; 3Department of Molecular and Developmental Medicine, University of Siena, Siena, Italy; 4Department of Hygiene and Epidemiology, “Santa Maria alle Scotte” Teaching Hospital, Siena, Italy
Abstract
Background: Operating theatres (OTs) have adequate conditions to perform safe operations and to prevent surgical site infections (SSIs). Opening doors can compromise these situations. Measurement of particulate contamination is a crucial point to check the effectiveness of preventive measures in the OTs. We analysed how opening the doors interact with particulate contamination in different designs of OTs.
Methods: Between January and February 2020, a cross-sectional study was conducted in five different types of OTs of a teaching hospital in Siena. Two (OTs 1 and 2) had laminar flows, with 58 and 55 air changes/h, respectively. Three had turbulent flows: OT3 (18 air changes/h, with four inlets from the ceiling), OT4 (16 air changes/h, airflow directed from one wall to the opposite one and the main door laterally to the flow) and OT5 (23 air changes/h and airflow from the ceiling plenum). Particulate matter (PM) measurements were carried out at seven different locations in each OT, alternating two conditions: 1) doors closed and 2) opening/closing the main door twice per minute. For each spot, in each condition, we recorded for several minutes the following parameters: particles (>0.3, >0.5, >1, >3, >5 and >10 µm), room temperature (RT), relative humidity (RH) and airflow velocity (AS). International Organization for Standardization (ISO) class for PM > 0.5 µm was calculated. Comparison with the Wilcoxon signed-rank test was made using Stata 16 (StataCorp LLC, College Station, TX, USA).
Results: All five OTs had differential pressure, but all fell to 0 at door opening; negligible changes were detected on microclimatic parameters although they may be affected by different types of airflows and design. Even though the variations in the turbulent flow rooms were broader and different, there were no changes in ISO class particle classification, given the already very high initial particulate levels. In laminar flow rooms, with a better ISO classification, the variations were smaller but sufficient to worsen the class.
Conclusions: When opening the doors, the PM levels in OTs are influenced by different ventilation systems and room design. Different ventilation systems and the design of OTs influence particulate levels during door opening. Particulate variations in the laminar flows studied were smaller than in the turbulent flows, which, although lower in performance in our study, can be just as effective; however, as the heterogeneous construction and logistic characteristics of OTs result in significant variations in PMs, further research is needed to determine the actual effect of airflow on the SSI rate.
Keywords: particulate matter; operating rooms; controlled environment; ventilation; laminar flow; turbulent flow
Citation: Int J Infect Control 2022, 18: 22156 – http://dx.doi.org/10.3396/ijic.v18.22156
Copyright: © 2022 Alessandro Della Camera et al. This is an Open Access article distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for any purpose, even commercially, provided the original work is properly cited and states its license.
Received: 25 October 2021; Revised: 1 March 2022; Accepted: 21 July 2022; Published: 13 October 2022
Competing interests and funding: The authors declare no conflict of interest.
This research was partly funded by Aerobiotix Inc. (Dayton, OH, USA). The sponsor was not involved in study design, data collection, analysis or interpretation, the paper’s writing or the decision to publish the results.
*Gabriele Messina, University of Siena, Via Aldo Moro 2, Siena, phone: 3396699422. Email: gabriele.messina@unisi.it
Highlights
- We present how the opening of the door affects particulate matter in operating theatres.
- The performance of operating rooms depends on their construction characteristics, which must be designed according to the type of surgical procedures to be performed.
- Laminar flows investigated were less influenced than turbulent flows.
- The potentially damaging effects caused by opening the door can only be accurately assessed through precise and continuous direct measurements of the combination of all parameters of the room.
Introduction
According to the European Centre for Disease Prevention and Control, surgical site infections (SSIs) are the most common healthcare-associated infections (HAIs), with a percentage varied from 0.5 to 10.1% for different surgical procedures. They increase mortality, postoperative hospital stays, additional surgical procedures, treatment in intensive care units and cost (1). In European countries, SSIs represent a considerable economic burden although comparing costs between countries, and averaging them is not easy (2).
Multiple approaches and recommendations have been considered in preventing the risk of SSI; the control of the operating theatre (OT) environment is one of them (3). OTs are designed to offer safe conditions for surgery and to prevent SSIs. Many factors related to design, construction, renovation and maintenance may compromise the safety of the OTs. OT parameters, such as air turnover, type of flow, pressure gradient between the OT and the outside, air particle amount and microbiological contamination of surface and air, are regulated by national and regional laws (4), national guidelines (5) and multiple International Organization for Standardization (ISO) guidelines as briefly described in the Methods.
The role of the type of flows, turbulent and laminar, for reducing SSI in OTs is still widely debated, with a particular focus on prosthetic surgery (3). A recent meta-analysis found no benefit of laminar airflow over turbulent ventilation in reducing the risk of SSI in total hip and knee arthroplasties and abdominal surgery (6). Another study evaluated the cost-effectiveness of laminar airflow systems for total shoulder arthroplasty, concluding that to justify the installation and maintenance costs of this technology, a high number of total shoulder arthroplasty with a high reduction in periprosthetic joint infection rates are required (7). A multicentre study found that there was a significant relation between the turbulent ventilation system and particle counts with increased air microbial counts, but not with wound contamination (8). Measures to increase OT air turnover can ensure a reduction in the number of particles and the bacterial load in the room (9). However, sometimes the desired result is not achieved with an increase in energy consumption and costs (10).
Door openings have an impact on air quality. The positive air pressure of the OT should prevent contamination by outside air, but under certain conditions, this can be cancelled or reversed by opening the door and failing OT prevention measures, with an increase in bacteria and airborne particles (11–13). Although a strong relationship among air contamination, microbial contamination and SSI is still debated, it is logical to assume that airborne particles may be potential carriers of pathogenic bacteria and an additional potential cause of SSI. Electronic particle counting can be taken as an objective measure of the efficacy of air systems in OTs and a predictor of the risk of SSI (8, 14).
This research aims to evaluate particulate matter (PM) and microclimatic variations resulting from the door opening in different types of OTs.
Methods
Setting
Between December 2019 and February 2020, a cross-sectional study compared levels of airborne particulate, differential pressures and microclimatic parameters in five different types of OT, at a teaching hospital of Siena, in the following two experimental conditions: 1) doors closed and 2) opening/closing of the main door. The entire opening and closing operation lasted 25 s: the door remained open for 10 s and the opening/closing movement lasted 15 s. The opening/closing was run twice. The recording period was defined within 6 min to ensure that any measurements would cease to vary. Temporal data were recorded with a sampling time of 1 min. The PM and other parameters were recorded in seven locations for each room, alternating the two studied conditions.
A portable particle counter, Climet Ci-550 (Climet Instruments Company, Redlands, CA, USA), was used for the detection of different particle sizes: diameter >0.3, >0.5, >1, >3, >5 and >10 µm. The Climet filter was cleaned before each measurement, and 30 L of air was sampled each time. A microclimate datalogger Delta OHM HD 32.3 with relative humidity (RH) and temperature combined probe HP3217.2R, omnidirectional hotwire probe AP3203.2 and globe temperature probe TP3276.2 (Delta OHM S.r.l., Caselle di Selvazzano (PD), Italy) was used to record air temperature (RT), RH and airflow velocity (AS). It was placed at about 15 cm to the left of the Climet particle counter and was used to measure microclimatic parameters. The seven sampling locations were as follows: in the centre of the operating table, at the four corners of the OT, near a window if present and near the main door. Differential pressure (∆P) between the OT and the adjacent room through the main door was measured with a manometric control unit Testo 420 (Testo SE and Co. KGaA, Titisee-Neustadt, Germany). We particularly focused during the analysis on PM > 0.3 and PM > 0.5 because these are cumulative of all the larger particles, and because they are the particle sizes that are most commonly considered for the classification of rooms and the cleanliness recovery performance test (15, 16).
Experimental sites
The first experimental phase (Phase 1) was conducted to optimise the project in the Department of Molecular Medicine and Development laboratories at the University of Siena. Reports and technical data of each OT were used to choose the study setting and to organise further stages. Specifically, the influence of the positioning of the instrument on the measurements was evaluated. The second stage (Stage 2) of the study was carried out in five different OTs of the Teaching Hospital of Siena: two had laminar, and three had turbulent airflow systems.
The OTs had the usual furnishings: an operating table with an anaesthesia column at its head, operating lamps over the table, an instrument table, medical device trolleys and other furniture around the walls of the room. The particle counter was placed on a Mayo table. The measurements were taken when the rooms were at rest, i.e. the installation is complete with equipment installed, and no surgery was taking place. However, two operators were always present in the rooms to take measurements.
The OTs meet national and regional standards (4, 5), which refer to ISO guidelines. These guidelines also regulate the frequency and methods of verifications. OTs are periodically examined by our team according to these regulations. From these inspection reports, some parameters have been extracted, such as the air turnover, measured, however, just before the study.
We briefly mention some of the technical requirements (reference limits) that we have touched upon in our work:
- Particle contamination: ISO classification (UNI EN ISO 14644-1) (15) was used to describe air cleanliness in suspended particles, where ISO 1 indicates the cleanest room and ISO 9 the dirtiest one. For OTs with a very high relative sterility requirement (e.g. transplants, cardiac surgery, orthopaedics and neurosurgery), at least ISO class 5 is required, measured under the necessary unidirectional flow, while for other theatres, at least ISO class 7 is required, even with non-unidirectional flow (5, 15, 16).
- Air filtration: 99.97%.
- Microclimatic: air temperature: 20°C–24°C; RH: 40–60%; AS: should not cause harm to exposed personnel and should, therefore, be kept as low as possible (not less than 0.05 m/s) as a precautionary measure. Fanger indices for the ‘thermal comfort’ of the worker (reference limits: predicted mean vote or PMV: ± 0.5; predicted percentage of the dissatisfied, PPD: < 10%) were not considered in this study.
- Air turnover: minimum of 15 changes per hour. Measurement method also refers to EN ISO 14644-3 (16).
- Positive pressure difference: the minimum pressure difference to less clean adjacent rooms to prevent the ingress of dirty air must be at least 5 Pa (UNI EN ISO 14644-4:2004) (17).
Operating theatres
All OTs are equipped with a specialty area (the pre-operating room) that is staffed by perianaesthesia nurses who provide nursing assessment, monitoring and document verification of pre-operative procedures. Moreover, an area for hand washing is always closed to the OTs.
OT1 is a cardiac surgery theatre, 110 m3 in volume, with a laminar airflow system; it was classified ISO 5 by the project. Air turnover per hour was about 58 m3/h, and the positive pressure difference (∆P) at the main door was 31 Pa. There is the main clean air inlet (plenum about 3 × 3 m) in the ceiling over the operating table (M1) and five outlets (R1–5), three (R1–2A/B) in the wall opposite to the main door and two (R3–4, together about 3 × 1.2 m) in the ceiling near the door. A vertical plexiglass panel was designed by the project and installed to separate the inlet and outlet airflows between M1 and R3–4 (Fig. 1, OT1; Table 1). The theatre has the main door from the pre-operating room and a utility door to semi-restricted corridor with scrub sinks, both separated by another door from the main atrium of the operating ward, where all other rooms are accessible. In OT1, two guillotine windows allow one the entrance of the kits for the intervention and the other the exit of the material used.

Figure 1. Images of the five operating theatres (OTs) studied. Refer to text for descriptions.
OT2 is an orthopaedics OT, 141 m3 in volume, with a laminar airflow system; it was classified ISO 5 by the project. Air hourly turnover was about 55 m3/h, and ∆P at the main door was 30 Pa. There is the main air inlet (plenum about 3 × 3.6 m, M1–8) in the ceiling over the operating table and eight air outlets in the four corners of the room (R1–4) (Fig. 1, OT2; Table 1). The theatre has a main door from the pre-operating room, separated by another door from the main atrium of the operating ward, and there is a guillotine window connecting with a utility room. The pre-operating area serves two OTs, including OT2.
OT3 is placed in a zone serving four theatres that share the same pre-operating area where operators also perform hand washing; the one tested is a general surgery OT of 102 m3 in volume, with a turbulent airflow system and classified as classified as ISO 7 by the project. Air turnover was about 18 m3/h, and ∆P at the main door was 11.5 Pa. There are four inlet vents placed in the ceiling and eight outlet vents, two per corner (Fig. 1, OT3; Table 1). The theatre has two doors; the main one connects the pre-operating room; the second one connects a corridor, running all around the four OTs of the operating plate, to remove used instruments.
OT4 is a gynaecology OT with a turbulent airflow system, 123 m3 in volume; it was classified ISO 7 by the project. Air turnover was about 16 m3/h, and ∆P at the main door was 31 Pa. There are nine air inlets (M1–9) in the right wall at the ceiling level. They are directed slightly downward, and there are four outlets (R1A/B–R2A/B) in the opposite wall (Fig. 1, OT4; Table 1). The theatre has the main door connected to its pre-operating room and a utility door to its hand washing area. The pre-operating and hand washing areas also have doors that separate the operating ward’s main atrium, where all other rooms are accessible. In OT4, there are also two guillotine windows connecting with a dirty and a clean room, respectively.
OT5 is an emergency OT, 105 m3 in volume, with a turbulent airflow system; it was classified as ISO 7 by the project. Air turnover was about 23 m3/h, and ∆P at the main door was 11 Pa. In the ceiling, over the operating table are placed the air inlets (plenum about 2.5 × 1.8 m, M1–6); eight air outlets (R1A/B–R4A/B) are positioned in the four corners of the room (Fig. 1, OT5; Table 1). The theatre has two doors: the main one separates the main atrium of the operating ward, and the second one separates the pre-operating room. There is also a storage room without a door, but an air inlet (Ma) and outlet (Ra) and guillotine window connecting with a utility room.
Statistical analysis
The descriptive statistics are reported as a median and interquartile range for particle counts and mean ± standard deviation for physics parameters. The ISO class of the operating rooms for particles larger than 0.5 µm was evaluated by calculating the upper confidence limit (UCL) with the formula: average + t*SE, where t is the Student’s t factor and SE is the standard error according to ISO 14644-1 (15). Depending on whether the distributions of the quantitative variables (parameters studied) were normally or non-normally distributed, the Student t-test or the Wilcoxon signed-rank test was, respectively, used to compare the corresponding data pairs. Normality was tested with the Shapiro-Wilk test. Differences were considered at a statistically significant level of 95% (P < 0.05).
The particle variations were analysed separately for PM > 0.3 and PM > 0.5 and for the two measurement conditions (door closed and during openings) for all analyses described below. Using the Wilcoxon signed-rank test, by pairing the measurement values for the seven points and six times, the operating rooms were compared in pairs first for absolute values and then for absolute and percentage variations. The last comparison allowed the evaluation of differences in time behaviour, independently from the number of particles. To complete this last analysis for each OT, Kendall’s rank correlation (P < 0.05) between the median of the particles and the measurement time was performed.
Finally, the analysis for the different room measurement points was made in each room by comparing the paired values in the two measurement conditions (door closed and during openings).
The Stata/SE ver 16.0 software (StataCorp LLC, College Station, TX, USA) was used to run statistical analysis. Databases and graphs were produced using Microsoft Excel 2016 software (Microsoft Corporation, Redmond, WA, USA).
Results
In all OTs, the differential pressure measured at the main door dropped to 0 in 1–2 s each time the door was opened.
All OTs had significantly different particulate levels except for the two laminar rooms for both particle sizes during the door opening and closing phase, and OT4 compared to OT3 for PM > 0.3 with the door closed and OT5 for PM > 0.5 during the opening phase. For both particle sizes, all absolute variations were significantly different except for all three comparisons between OT5 and the two laminar OT1 and OT2, while the analysis of the percentage variations showed a significant difference between OT4 and all other OTs and between OT3 and OT5.
In Figs. 2 and 3, it is possible to observe that for both PM > 0.3 and PM > 0.5, the OTs with turbulent flows had higher particulate levels than the laminar ones. Among them, OT3 had the highest particulate values (shown on a secondary y-axis in Figs. 2 and 3); for both particle sizes, there is a significant decrease in particles over time with the door closed, and, conversely, an increase with the door openings. The UCL for PM > 0.5 increased from 4690.5/m3 to 22133.4/m3 between the two measurements conditions. It was classified in ISO class 6 for the PM > 0.5, while OT4 and OT5 were classified in ISO 5. OT4 particulate levels decreased slightly over time with the door closed; in addition, opening and closing the door produced a further reduction, with the UCL for PM > 0.5 declining from 2318.9/m3 to 1986.26/m3. OT5 had the lowest values among OTs with turbulent flow; opening and closing the door produced a slightly increase of PM. However, in practice, the ISO classifications of OT4 and OT5 did not deteriorate between the two conditions.
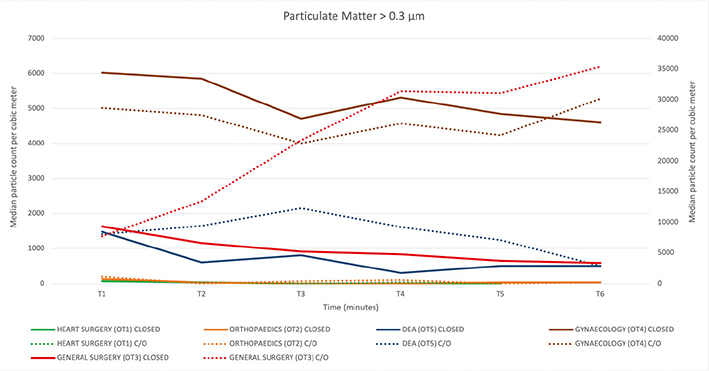
Figure 2. Representation of particle matter >0.3 μm. The 6 min of the recording is shown in the X-axis, while the Y-axis shows the median values of the seven sampling points. C/O = opening and closing operation. OT3 closed, and C/O are reported on the right Y-axis.
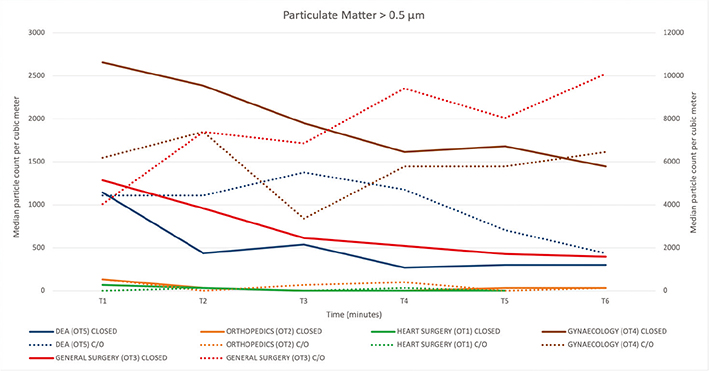
Figure 3. Representation of particle matter >0.5 μm. The 6 min of the recording is shown in the X-axis, while the Y-axis shows the median values of the seven sampling points. C/O = opening and closing operation. OT3 closed, and C/O are reported on the right Y-axis.
On the other hand, the laminar rooms had minimum particulate values. The recorded data and values were consistent with ISO 4 classification for PM > 0.5 with minimum variations with the door’s opening, which, however, involved a change to the lower class. The UCL for PM > 0.5 increased from 98.3/m3 to 461.6/m3 in OT1 and from 222.6/m3 to 609.2/m3 in OT2. However, in OT1 the ISO class did not change when calculated under laminar flow.
The analysis for each measurement site is shown in Fig. 4; only statistically or borderline significant results are reported. In particular, in OT1, the only variations were detected at location 6 with an increase both for PM > 0.3 and PM > 0.5; in OT2, an increase in PM > 0.3 and PM > 0.5 at locations 4 and 7; in OT3, an increase of both particle counts at the points closest to the doors and the anaesthesia column; in OT4, a reduction in counts was detected in some points on the surgical bed; in OT5, a reduction of PM > 0.5 (able to improve ISO class when considering single points) in location 7 and an increase in both particles in location 6.
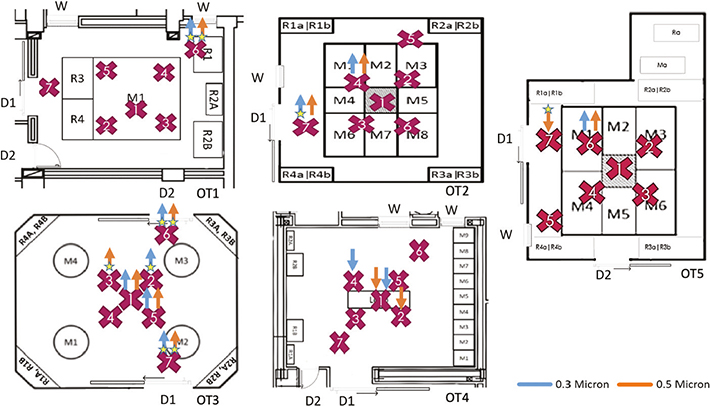
Figure 4. Analysis by sampling location, purple cross. Only significant (P < 0.05) or borderline significant ★ (P = 0.0625) variations are indicated. Blue and orange arrows indicate increase or decrease in particle matter. M = air inlet; R = air outlet; a = high on the wall; b = down on the wall; D1 = main door; D2 = secondary door; W = window.
Changes in microclimatic parameters occurred mainly with AS that decreased on average from 0.07 ± 0.06 to 0.05 ± 0.04 m/s in OT3, and rose in OT5 from 0.07 ± 0.09 to 0.09 ± 0.08 m/s.
Discussion
Door openings in OTs are correlated with PM levels and airborne microbial load. Although the results of all prior studies are not always consistent, it is agreed that reducing door openings and the comings and goings of OT staff are strategies in the control of SSIs. Laminar airflow systems can protect against the negative influence of high OT staff numbers and door openings (12, 18, 19).
Due to construction characteristics, the five OTs studied here have different airflows: OT1 and OT2 have laminar airflow systems with different dynamics and a very high hourly air turnover. The latter can explain why particle counts were close to zero; any spike could be attributed to proximity to furniture or the door. For example, in OT1, the PM counts at the sampling location furthest from the door (near the sealed window) tended to increase when the door was opened and closed. The laminar airflow from the air inlet and the high air turnover keeps PM low and unaffected by the door opening. In OT2, the sampling location showing the greatest increase in PM was close to the main door, away from the air inlet. Another sampling location, just below the inlet to one side of the door, was affected by the door opening such that the ISO class deteriorated. In any case, there were no critical points in the OT or around the operating table. This is probably due to the laminar airflow and high air turnover.
OTs 3, 4 and 5 have turbulent airflow systems with different dynamics. In OT3, we found the widest variation in PM during door opening/closing in 6 of 7 sampling locations. This could be partly due to differences in air flow systems and pressure, although excess furniture could play a role. However, this should not be ignored in the endeavour to reduce the probability of SSIs. OT4 had airflow directed from one wall across the OT. The air inlet is close to the ceiling and is directed slightly downward; the air intake grills are in the opposite wall. The windows and doors are on the other two walls, near the inlet and outlet, respectively. Air turnover was less than in OT3 and OT5, but the differential pressure at the main door was very high (∆P 31 Pa). This could lead to air cleaning during door opening. Three locations on the operating table showed a significant reduction in particles during door opening. It seems that the high-pressure difference functions well when the door is opened and creates a significant reduction in PM on the operating table. In OT5, there was a contrasting variation near the door. The PM count decreased at the door and increased at the point of the bed closest to the door. This could be due to an increase in turbulent flow created by the opening of the door.
Not surprisingly, we found that rooms with laminar airflow had a better ISO class with much lower particulate levels in both conditions than rooms with turbulent airflow. In general, OTs with laminar airflow systems had a lower ISO class. Although absolute values change very little, it was sufficient to cross the PM threshold between ISO 4 and 5 classes. However, we have to remember that these OTs were designed to be ISO 5, so our determination of ISO 4 was better than expected. In OTs with turbulent airflow, PM variations were wider. It must be considered that OTs with laminar flow systems have a higher air turnover than those with turbulent flow systems, and this influences air quality (9).
Analysis of different sampling locations seemed to show that peripheral sampling points generally seemed to be more affected by increases in PM counts, likely due to the presence of the door or furniture.
Some microclimatic parameters showed significant changes between the two conditions (P < 0.05) in OTs 1, 3 and 5. However, the changes were so small that they could be ignored to study the PM. In addition, although the two or three OT staff involved in the simulations did not experience discomfort, a greater number of theatre staff may influence microclimatic parameters and the level of discomfort.
The frequency and duration of door opening can modify positive room pressure. Previous experimental studies and software simulations have shown that repeated door opening can cancel or reverse the positive pressure in the OT, altering the safety of the operating environment (11, 12). The time necessary to restore safe conditions presumably also depends on OT characteristics. It was not evaluated in the different OTs, but it is reasonable to suppose it would be briefer in theatres with laminar airflow systems.
The positive pressure differential, the type of door (sliding or swinging, width and direction of opening) and the passage of staff and materials through the door may also influence pressure variations (20). In this study, all the doors were sliding with manual or automatic opening, and an attempt was made to standardise the opening time.
Finally, we found that OTs with laminar airflow systems were less influenced by door openings than those with turbulent airflow. The great variability found in the latter case was due to their construction characteristics. New OTs with turbulent airflow systems could achieve better ISO ratings and be just as effective in maintaining low PM levels in all conditions if designed, installed and maintained correctly. Since this is not always the case, recording the number of times there is a pressure change in the OT can be useful for detecting a change in PM with possible undesirable consequences. The number of pressure changes and PM variations could be monitored together with other factors to verify possible associations with adverse events such as SSIs.
The study has some limitations. The detected parameters and PM levels were studied under repeatable conditions, but different situations may produce different results during a real surgical procedure. Movement of operators and suboptimal behaviour of the staff are certainly to be considered as these have adverse effects on the dynamics of the flows and particle counts. Clothing also influences the number of particles produced and the dispersion of skin bacteria (21).
Continuous monitoring of PM could be used to check for significant variations with opening or closing of doors and estimate the likelihood of adverse outcomes due to different PM sizes and quantities. Paradoxically, an environment with high levels of PM where there is no significant variation in PM during door opening and closing may pose a higher risk of SSIs than environments where there is a significant variation in barely detectable quantitative levels. For this reason, if an SSI risk equation were to be defined, the combination of all parameters should certainly be considered.
Conclusions
The construction features of OTs, including air dynamics, airflow (laminar or turbulent) and door position, can result in significant differences in PM variations when opening the door. Although PM levels differ significantly between rooms with laminar and turbulent airflow systems, the potentially harmful effects caused by door opening can only be accurately assessed through precise direct measurements, such as measuring microbiological air contamination and infection rates. Therefore, further investigations are needed to determine the actual effect of airflow on the SSI rate.
Author contributions
Conception, methodology and supervision: GM, GC, MDM and NN; investigation: ADC and GM; formal analysis: ADC and GM; writing-original draft: ADC, GM, GC, MDM and NN; writing-review and editing: ADC, GM and GC.
Acknowledgements
The authors thank the Teaching Hospital of Siena for conducting the study in the structure.
Ethics statement
The Teaching Hospital Directorate authorized the study. No Ethics statement is required since no subjects were involved in the study.
References
| 1. | European Centre for Disease Control. Healthcare-associated infections: surgical site infections – annual epidemiological report for 2017. Stockholm: European Centre for Disease Prevention and Control; 2019. Available from: https://www.ecdc.europa.eu/en/publications-data/healthcare-associated-infections-surgical-site-infections-annual-1 [cited 18 June 2020]. |
| 2. | Badia JM, Casey AL, Petrosillo N, Hudson PM, Mitchell SA, Crosby C. Impact of surgical site infection on healthcare costs and patient outcomes: a systematic review in six European countries. J Hosp Infect 2017 May; 96(1): 1–15. doi: 10.1016/j.jhin.2017.03.004 |
| 3. | World Health Organization. Global guidelines for the prevention of surgical site infection, second edition. Geneva: World Health Organization; 2018. Licence: CC BY-NC-SA 3.0 IGO. Available from: https://www.ncbi.nlm.nih.gov/books/NBK536404/ [cited 6 July 2020]. |
| 4. | Decree of the President of the Republic of 14 January 1997 – approval of the act of address and co-ordination to the regions and autonomous provinces on the subject of minimum structural, technological and organisational requirements for the exercise of healthcare activities by public and private structures. G.U. n. 42 of 20 February 1997 – ordinary supplement. Available from: https://www.gazzettaufficiale.it/eli/id/1997/02/20/097A1165/sg [cited 21 February 2022]. |
| 5. | Istituto Superiore Per La Prevenzione E La Sicurezza Del Lavoro (Ispesl) – guidelines on standards of safety and hygiene at work in the operating ward; translated from ‘Linee Guida Sugli Standard Di Sicurezza E Di Igiene Del Lavoro Nel Reparto Operatorio’. ISPESL; 2009. Available from: https://www.inail.it/cs/internet/docs/linee-guida-igiene-reparto-operatorio.pdf?section=attivita [cited 15 February 2022]. |
| 6. | Bischoff P, Kubilay NZ, Allegranzi B, Egger M, Gastmeier P. Effect of laminar airflow ventilation on surgical site infections: a systematic review and meta-analysis. Lancet Infect Dis 2017; 17(5): 553–61. doi: 10.1016/S1473-3099(17)30059-2 |
| 7. | Davis ED, Zmistowski B, Abboud J, Namdari S. Cost effectiveness of laminar flow systems for total shoulder arthroplasty: filtering money from the OR? Arch Bone Jt Surg 2020 1; 8(1): 38–43. |
| 8. | Birgand G, Toupet G, Rukly S, Antoniotti G, Deschamps M-N, Lepelletier D, et al. Air contamination for predicting wound contamination in clean surgery: a large multicenter study. Am J Infect Control 2015; 43(5): 516–21. doi: 10.1016/j.ajic.2015.01.026 |
| 9. | Vonci N, De Marco MF, Grasso A, Spataro G, Cevenini G, Messina G. Association between air changes and airborne microbial contamination in operating rooms. J Infect Public Health 2019 Dec; 12(6): 827–30. doi: 10.1016/j.jiph.2019.05.010 |
| 10. | Gormley T, Markel TA, Jones H, Greeley D, Ostojic J, Clarke JH, et al. Cost-benefit analysis of different air change rates in an operating room environment. Am J Infect Control 2017 Dec 1; 45(12): 1318–23. doi: 10.1016/j.ajic.2017.07.024 |
| 11. | Sadrizadeh S, Pantelic J, Sherman M, Clark J, Abouali O. Airborne particle dispersion to an operating room environment during sliding and hinged door opening. J Infect Public Health 2018; 11(5): 631–5. doi: 10.1016/j.jiph.2018.02.007 |
| 12. | Weiser MC, Shemesh S, Chen DD, Bronson MJ, Moucha CS. The effect of door opening on positive pressure and airflow in operating rooms. J Am Acad Orthop Surg 2018; 26(5): e105–13. doi: 10.5435/JAAOS-D-16-00891 |
| 13. | Smith EB, Raphael IJ, Maltenfort MG, Honsawek S, Dolan K, Younkins EA. The effect of laminar air flow and door openings on operating room contamination. J Arthroplasty 2013; 28(9): 1482–5. doi: 10.1016/j.arth.2013.06.012 |
| 14. | Messina G, Spataro G, Catarsi L, Francesca De Marco M, Grasso A, Cevenini G, et al. A mobile device reducing airborne particulate can improve air quality. AIMS Public Health 2020; 7(3): 469–77. doi: 10.3934/publichealth.2020038 |
| 15. | International Organization for Standardization (ISO). International Standard ISO 14644-1:1999. Cleanrooms and associated controlled environments – Part 1: classification of air cleanliness. Geneva, Switzerland; 1999 (revised in 2015) |
| 16. | International Organization for Standardization (ISO). International Standard ISO 14644-3:2005. Cleanrooms and associated controlled environments – Part 3: test methods. Geneva, Switzerland; 2005 (revised in 2019) |
| 17. | International Organization for Standardization (ISO). International Standard ISO 14644-4:2001. Cleanrooms and associated controlled environments – Part 4: design, construction and start-up; Geneva, Switzerland; 2001 |
| 18. | Rezapoor M, Alvand A, Jacek E, Paziuk T, Maltenfort MG, Parvizi J. Operating room traffic increases aerosolized particles and compromises the air quality: a simulated study. J Arthroplasty 2018; 33(3): 851–5. doi: 10.1016/j.arth.2017.10.012 |
| 19. | Scaltriti S, Cencetti S, Rovesti S, Marchesi I, Bargellini A, Borella P. Risk factors for particulate and microbial contamination of air in operating theatres. J Hosp Infect 2007 Aug; 66(4): 320–6. doi: 10.1016/j.jhin.2007.05.019 |
| 20. | Hendiger J, Chludzińska M, Ziętek P. Influence of the pressure difference and door swing on heavy contaminants migration between rooms. PLoS One 2016; 11(5): e0155159. doi: 10.1371/journal.pone.0155159 |
| 21. | Mitchell NJ, Evans DS, Kerr A. Reduction of skin bacteria in theatre air with comfortable, non-woven disposable clothing for operating-theatre staff. Br Med J 1978; 1(6114): 696–8. doi: 10.1136/bmj.1.6114.696 |