ORIGINAL ARTICLE
Rates of urinary catheter-associated urinary tract infection in Saudi MOH hospitals: a 2-year multi-centre study
Yvonne S. Aldecoa1, Adel Alanazi1, Ghada Bin Saleh1, Nasser Alshanbari1, Tabish Humayun1*, Faisal Alsheddi1, Aiman El-Saed2, Mohammed Alqahtani1 and Khalid H. Alanazi1
1Surveillance Department, General Directorate of Infection Prevention and Control (GDIPC), Ministry of Health (MOH), Riyadh, Kingdom of Saudi Arabia; 2Infection Prevention and Control Department, King Saud bin Abdulaziz University for Health Sciences, Riyadh, Kingdom of Saudi Arabia
Abstract
Background: The published rates of catheter-associated urinary tract infection (CAUTI) in Saudi Arabia were derived from single-centre studies or nationally non-representative studies.
Objectives: The aim of this study was to estimate CAUTI rates and urinary catheter utilisation (UCU) ratios in 99 Saudi Ministry of Health (MOH) hospitals from all regions.
Methods: A prospective surveillance study was conducted in 15 different types of intensive care units (ICUs) between January 2018 and December 2019. The data were entered into the Health Electronic Surveillance Network (HESN) programme. The methods of the US National Healthcare Safety Network (NHSN) and the Gulf Cooperation Council (GCC) centre for infection control were used.
Results: During 2 years of surveillance covering 919,615 patient-days and 573,720 urinary catheter days, a total of 965 CAUTI events were identified. The overall MOH CAUTI rate was 1.68 (95%confidence interval (CI) 1.58–1.79) per 1,000 urinary catheter days, and the overall UCU was 0.624 (95%CI 0.623–0.625). CAUTI rates were highest in paediatric medical (5.73) and adult medical (2.02) ICUs. UCU were highest in neurosurgical (0.795) and medical surgical (0.743) ICUs. CAUTI standardised infection ratios across different ICUs in Saudi MOH hospitals were 16% lower than NHSN hospitals, 47% lower than GCC hospitals and 69% lower than International Nosocomial Infection Control Consortium (INICC) hospitals. Urinary catheter standardised utilisation ratios across different ICUs in Saudi MOH hospitals were 15% higher than NHSN hospitals, 9% higher than INICC hospitals and 13% lower than GCC hospitals.
Conclusions: The current study is a unique national CAUTI benchmark that can potentially help in the fight against healthcare-associated infection.
Keywords: urinary catheters; catheter-associated infections; urinary tract infections; intensive care units; infection control; benchmarking; surveillance; Saudi Arabia
Citation: Int J Infect Control 2022, 18: 21703 – http://dx.doi.org/10.3396/ijic.v18.21703
Copyright: © 2022 Yvonne S. Aldecoa et al. This is an Open Access article distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for any purpose, even commercially, provided the original work is properly cited and states its license.
Received: 17 June 2021; Revised: 22 September 2021; Accepted: 30 September 2021; Published: 16 March 2022
Competing interests and funding: The authors report no conflicts of interest and funding in this work.
*Tabish Humayun, Surveillance Department, General Directorate of Infection Prevention and Control (GDIPC), Ministry of Health (MOH), PO Box: 11176, Riyadh, Kingdom of Saudi Arabia. Email: drtabish.ipc.micro.ph@gmail.com
The use of Foley’s catheter is an inevitable part of modern healthcare services, especially among intensive care patients, post-operative patients and neurological patients (1). Catheter-associated urinary tract infection (CAUTI) is one of the most frequent healthcare-associated infections (HAIs), representing up to one-third of all HAIs (2–4). CAUTI events cause approximately 10% excess mortality and approximately 10 days of additional stay among patients admitted to intensive care units (ICUs) (5, 6). In addition, they are the leading cause of secondary bloodstream infections (7, 8). Furthermore, CAUTI events are associated with disability, accounting for 16% of the total HAI-related years lived with disability (9). Moreover, they cause a significant increase in healthcare costs due to prolonged hospitalisation and associated morbidity (10).
Approximately 65–70% of the CAUTI events can be potentially prevented with appropriate infection prevention measures and control practices (11). The rate of CAUTI can be significantly reduced through implementation of preventive bundles in hospitalised patients (12). The results of HAI surveillance shared with healthcare providers is a key element of quality improvement and patient safety (13). In addition, CAUTI surveillance with or without other preventive measures has been shown to reduce the utilisation of urinary catheters and the rate of CAUTI (14–16). The rates of CAUTI in Saudi Arabia have been estimated from several reports (17–20). However, some of these reports were derived from single-centre studies (19, 20), and none of them were nationally representative (17–20). Therefore, a national benchmark for CAUTI rates is still lacking. To overcome this, the Saudi Ministry of Health (MOH) started to collect standardised CAUTI data from its hospitals using the new system of health electronic surveillance network (HESN) programme. The objective of the current study was to estimate unit-specific CAUTI rates along with urinary catheter utilisation (UCU) ratios in MOH hospitals and, additionally, to benchmark such rates and ratios with recognised regional and international benchmarks.
Methods
Setting
The total number of hospitals in Saudi Arabia is 484, with a total bed capacity of approximately 75,000 beds. Of these, the MOH is administering 284 hospitals with a total bed capacity of around 43,000 beds (21). The current study was conducted in 99 Saudi MOH hospitals distributed in 20 different geographical regions across Saudi Arabia. Out of 99 hospitals, 86% were general or central hospitals, 9% were maternal and children’s hospitals, and 5% were cardiac hospitals (Table 1). The hospitals included in the CAUTI surveillance had a total bed capacity of 26,399 beds, including 3,560 ICU beds (Table 1).
Design
A prospective surveillance study was conducted between 1 January 2018 and 31 December 2019 using the HESN programme.
Population
All included hospitals had at least 100-bed capacity, one ICU, a microbiology laboratory and a full-time microbiologist. The data were obtained from 15 different types of ICUs. The data were included in the analysis if at least 50 urinary catheter days of surveillance were reported per the reporting year, 2018 or 2019 (Table 2).
| Type of ICU | Number of ICUs* | Urinary catheter days | CAUTI events | Mean CAUTI rate | 95% Confidence interval | Percentile** | ||||
| 10% | 25% | 50% (median) | 75% | 90% | ||||||
| Burn | 8 | 3,253 | 5 | 1.54 | 0.19–2.88 | |||||
| Medical | 47 | 73,600 | 149 | 2.02 | 1.70–2.35 | 0.00 | 0.00 | 1.06 | 3.45 | 5.41 |
| Medical cardiac | 29 | 20,344 | 20 | 0.98 | 0.55–1.41 | 0.00 | 0.00 | 0.00 | 1.51 | 2.19 |
| Medical surgical | 161 | 420,588 | 724 | 1.72 | 1.60–1.85 | 0.00 | 0.00 | 0.94 | 2.49 | 4.28 |
| Neurological | 2 | 289 | 0 | 0.00 | 0.00–0.00 | |||||
| Neurosurgical | 3 | 6,156 | 11 | 1.79 | 0.73–2.84 | |||||
| Paediatric cardiothoracic | 2 | 428 | 0 | 0.00 | 0.00–0.00 | |||||
| Paediatric medical | 10 | 4,883 | 28 | 5.73 | 3.61–7.86 | |||||
| Paediatric medical surgical | 38 | 22,312 | 16 | 0.72 | 0.37–1.07 | 0.00 | 0.00 | 0.00 | 0.89 | 5.67 |
| Paediatric surgical | 2 | 505 | 0 | 0.00 | 0.00–0.00 | |||||
| Prenatal | 1 | 54 | 0 | 0.00 | 0.00–0.00 | |||||
| Respiratory | 3 | 2,300 | 0 | 0.00 | 0.00–0.00 | |||||
| Surgical | 9 | 10,679 | 5 | 0.47 | 0.06–0.88 | |||||
| Surgical cardiothoracic | 5 | 3,915 | 3 | 0.77 | 0.00–1.63 | |||||
| Trauma | 4 | 4,414 | 4 | 0.91 | 0.02–1.79 | |||||
| Total | 324 | 573,720 | 965 | 1.68 | 1.58–1.79 | 0.00 | 0.00 | 0.46 | 2.18 | 4.23 |
| *ICUs contributing less than 50 urinary catheter days per year were excluded from the analysis. **Standard percentiles were calculated only when at least 20 hospitals were contributing data for a specific type of ICU. |
||||||||||
Methods
The surveillance methodology was similar to the methods recommended by the US National Healthcare Safety Network (NHSN) (22) and the Gulf Cooperation Council (GCC) Centre for Infection Control (23). It was an active, patient-based, prospective targeted surveillance that was carried out in specific ICUs for specific durations after a local infection risk assessment.
Definitions
CAUTI was defined as a symptomatic urinary tract infection (SUTI) or an asymptomatic bacteremic urinary tract infection UTI (ABUTI) in a patient who had an indwelling urinary catheter. The catheter had to be in place for more than 2 days and in place at the date of CAUTI or the day prior. The symptoms included fever, suprapubic pain or tenderness, or costovertebral angle pain or tenderness, and additionally, urinary urgency, frequency or dysuria only if the catheter was not in place (22, 23). A physician’s diagnosis of UTI that did not match the surveillance criteria was not an acceptable diagnosis for CAUTI. The UCU, intended to provide a standardized indication of the extent of catheter use, was calculated by dividing the number of catheter-days by the number of patient-days in each participating ICU.
HESN programme
HESN is an integrated, semi-automated, national electronic surveillance system that has several domains to uniformly monitor communicable diseases, disease epidemics, immunisation and HAIs across Saudi Arabia (24). It allows users at different hospitals to continually and uniformly report HAIs to the General Directorate of Infection Prevention and Control (GDIPC) at Riyadh, Saudi Arabia. CAUTI and urinary catheter use data were collected by infection control practitioners (ICPs) at respective hospitals. The data were directly entered into the HESN programme at two levels: urinary catheter bundle form and CAUTI event form. The number of urinary catheter days was estimated using daily count at a fixed time (usually around 8.00 AM) for all patients with a urinary catheter or an electronic count that was within ±5% of the manually collected daily count. The surveillance department of GDIPC at MOH provided the included hospitals with the required training in surveillance definitions, surveillance methodology, use of HESN programme and information technology support. Training workshops followed by hands on training were conducted in all regions (during 2017) before the start of the study.
Statistical analysis
The data from all regions were extracted from the HESN programme and analysed using SPSS. Data extraction, management, analysis and interpretation were carried out centrally at the GDIPC. CAUTI rates (expressed per 1,000 urinary catheter days) and UCU ratios were calculated and stratified by type of ICU (18, 25). Confidence intervals (CIs) (18) and standard percentiles (25) were calculated for both CAUTI rates and UCU ratios. Percentiles were not calculated for ICU types with less than 20 data points (during a hospital year of surveillance). To benchmark the current CAUTI rates and UCU ratios with regional and international benchmarks, standardised infection ratios (SIRs) and standardised utilisation ratio (SUR) were calculated (respectively) after adjusting for differences in ICU types. SIR and SUR were calculated by dividing the number of observed CAUTI events and urinary catheter days (respectively) by their expected values (22). The expected values were calculated using the published reports of NHSN (25, 26), GCC (18) and International Nosocomial Infection Control Consortium (INICC) (27). P-values were two-tailed. P-value <0.05 was considered as significant. Statistical analyses were performed using SPSS software (release 25.0, Armonk, NY: IBM Corp.).
Results
During 2 years of surveillance covering 919,615 patient-days and 573,720 urinary catheter days, a total of 965 CAUTI events were identified. As shown in Table 2, the overall CAUTI rate was 1.68 per 1,000 urinary catheter days with 95%CI ranging between 1.58 and 1.79. The 50th, 75th and 90th percentiles were 0.46, 2.18 and 4.23, respectively. Five types of ICUs contributed 95% of the urinary catheter days surveyed in all types of ICUs: adult medical surgical, adult medical, paediatric medical surgical, adult medical cardiac and adult surgical. CAUTI rates per 1,000 urinary catheter days were highest in paediatric medical (5.73), adult medical (2.02), adult neurosurgical (1.79) and adult medical surgical (1.72) ICUs. There were no CAUTI events reported in adult respiratory, paediatric surgical, paediatric cardiothoracic, adult neurological and prenatal ICUs. The 90th percentiles of CAUTI rates per 1,000 urinary catheter days ranged from 2.19 in adult medical cardiac ICUs to 5.67 in paediatric medical surgical ICUs.
As shown in Table 3, the overall UCU ratio was 0.624, with the 95%CI ranging between 0.623 and 0.625. The 50th, 75th and 90th percentiles were 0.59, 0.78 and 0.88, respectively. The UCU ratios were highest in the following adult ICUs: neurosurgical (0.795), medical surgical (0.743), respiratory (0.724), trauma (0.723) and medical (0.715) ICUs. The UCU ratios were lowest in the following ICUs: adult burn (0.204), paediatric medical (0.211) and paediatric medical surgical (0.211) ICUs. The 90th percentiles of UCU ratios ranged between 0.45 in paediatric medical surgical ICUs and 0.91 in adult medical ICUs.
| Type of ICU | Number of ICUs* | Patient days | Urinary catheter days | Utilisation ratio | 95% confidence interval | Percentile** | ||||
| 10% | 25% | 50% (median) | 75% | 90% | ||||||
| Burn | 8 | 15,945 | 3,253 | 0.204 | 0.198–0.210 | |||||
| Medical | 47 | 103,007 | 73,600 | 0.715 | 0.712–0.717 | 0.40 | 0.54 | 0.72 | 0.87 | 0.91 |
| Medical cardiac | 29 | 61,642 | 20,344 | 0.330 | 0.326–0.334 | 0.19 | 0.26 | 0.36 | 0.47 | 0.72 |
| Medical surgical | 161 | 566,259 | 420,588 | 0.743 | 0.742–0.744 | 0.36 | 0.58 | 0.73 | 0.82 | 0.89 |
| Neurological | 2 | 562 | 289 | 0.514 | 0.473–0.556 | |||||
| Neurosurgical | 3 | 7,741 | 6,156 | 0.795 | 0.786–0.804 | |||||
| Paediatric cardiothoracic | 2 | 1,552 | 428 | 0.276 | 0.254–0.298 | |||||
| Paediatric medical | 10 | 23,106 | 4,883 | 0.211 | 0.206–0.217 | |||||
| Paediatric medical surgical | 38 | 105,868 | 22,312 | 0.211 | 0.208–0.213 | 0.06 | 0.10 | 0.15 | 0.30 | 0.45 |
| Paediatric surgical | 2 | 2,048 | 505 | 0.247 | 0.228–0.265 | |||||
| Prenatal | 1 | 184 | 54 | 0.293 | 0.228–0.359 | |||||
| Respiratory | 3 | 3,176 | 2,300 | 0.724 | 0.709–0.740 | |||||
| Surgical | 9 | 15,618 | 10,679 | 0.684 | 0.676–0.691 | |||||
| Surgical cardiothoracic | 5 | 6,801 | 3,915 | 0.576 | 0.564–0.587 | |||||
| Trauma | 4 | 6,106 | 4,414 | 0.723 | 0.712–0.734 | |||||
| Total | 324 | 919,615 | 573,720 | 0.624 | 0.623–0.625 | 0.13 | 0.34 | 0.59 | 0.78 | 0.88 |
| *ICUs contributing less than 50 urinary catheter days per year were excluded from the analysis. **Standard percentiles were calculated only when at least 20 hospitals were contributing data for a specific type of ICU. |
||||||||||
Figure 1 compares CAUTI rates and UCU ratios in adult and paediatric ICUs in MOH hospitals with other recognised benchmarking networks. CAUTI rates in adult ICUs in MOH hospitals were exactly the same as NHSN rates (1.7 each), lower than GCC rates (3.3), and much lower than INICC rates (5.3). CAUTI rates in paediatric ICUs in MOH hospitals (0.7) were lower than NHSN rates (2.5) and INICC rates (5.6). UCU ratios in adult ICUs in MOH hospitals (0.74) were slightly higher than NHSN ratios (0.60) and INICC ratios (0.62) but slightly lower than GCC ratios (0.85). UCU ratios in paediatric ICUs in MOH hospitals were exactly the same as NHSN ratios (0.21 each) and lower than INICC rates (0.31).
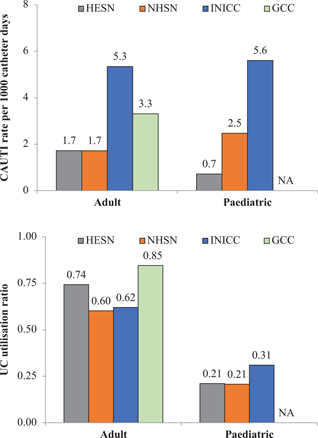
Fig. 1. Comparisons of CAUTI rates (above) and urinary catheter utilisation ratios (below) between the Saudi health electronic surveillance network (HESN) and other recognised benchmarking networks.
Note: Adult and paediatric ICUs were medical-surgical ICUs. NHSN, US National Healthcare Safety Network; INICC, International Nosocomial Infection Control Consortium of developing countries; GCC, Gulf Cooperation Council countries; CAUTI, catheter-associated urinary tract infection; UC, urinary catheter.
Table 4 compares CAUTI rates and UCU ratios in MOH hospitals with the three benchmarks using SIR and SUR, respectively. CAUTI SIR across all types of ICUs in MOH hospitals were significantly lower than the recognised benchmarks; 16% lower than NHSN hospitals, 47% lower than GCC hospitals and 69% lower than INICC hospitals. Urinary catheter SUR across all types of ICUs in MOH hospitals were 15% higher than NHSN hospitals, 9% higher than INICC hospitals and 13% lower than GCC hospitals.
Discussion
Using huge-standardised data, the current study is documenting CAUTI rates and UCU ratios in almost 100 Saudi MOH hospitals. The overall rate was 1.68 per 1,000 urinary catheter days. This rate is considered lower than CAUTI rates previously reported in Saudi Arabia (17–20). For example, CAUTI rates per 1,000 urinary catheter days ranged between 0.0 and 11.8 in ICUs of 12 referral and secondary MOH hospitals (17), between 1.3 and 4.1 in ICUs of four National Guard hospitals (18), and between 6.6 and 10.0 in three ICUs of Saudi Aramco Medical Services Organisation (19). The lower CAUTI rate in the current study can be explained by several factors. Firstly, the majority of previous local CAUTI data were collected based on the older CAUTI definition (18–20), while the current study used the new CAUTI definition. It has been shown that the new NHSN CAUTI definition introduced in 2015 resulted in a large reduction of CAUTI rates (7, 8). Secondly, some of the previous local CAUTI data were collected before widespread implementation of the urinary catheter bundle (18–20), whereas the current data were collected while the urinary catheter bundle was fully implemented. The implementation of the urinary catheter bundle resulted in a significant reduction of CAUTI rates (12). Thirdly, the majority of previous local CAUTI data were collected from one to three types of ICUs (17–20), while the current data were collected from 15 different ICUs, some of them had zero CAUTI rates. Finally, despite the training and auditing done by the GDIPC, under-reporting of CAUTI events to the new HESN system cannot be completely excluded.
The UCU ratio ranged between 0.20 and 0.80 with an average ratio of 0.62. The current UCU ratios are considered similar or slightly lower than those previously reported in Saudi Arabia (17–19). For example, UCU ranged between 0.06 and 0.85 in 12 MOH hospitals (17), between 0.39 and 0.69 in the Saudi Aramco Medical Services Organisation (19), and between 0.85 and 0.96 in four National Guard hospitals (18). The slightly lower UCU ratios in the current study may be related to the inclusion of paediatric ICUs in the current study but their exclusion in previous local reports (17–19). Paediatric ICUs in the current and international studies are known for their lower UCU ratios (25–27).
The current CAUTI rates were generally lower than the recognised international benchmarks, especially after adjusting for the type of ICUs. The difference was minimal with NHSN hospitals (25, 26) and considerable with INICC and GCC hospitals (18, 27). Similar to the local comparisons discussed above, the data used in these reports were mainly based on the older CAUTI definition and were collected before full implementation of the urinary catheter bundle (18, 27). Interestingly, the differences in UCU ratios between this study and recognised international benchmarks were minimal. The slightly lower urinary catheter SUR in MOH hospitals compared with GCC hospitals may be related to the presence of paediatric data in the current report but not the GCC report (18). The generally high UCU ratios in the current report and the recognised international benchmarks may indicate the need for more work to reduce catheter utilisation, including training and education (14, 15).
The current study can serve perfectly as a national benchmark for CAUTI. The benchmarking use of this study is supported by the large, unprecedented number of hospitals included, the coverage of 20 geographical regions, and the use of the same electronic data collection system. Additionally, this has been further facilitated by presenting unit-specific rates and ratios and by calculating CIs and standard percentiles for both rates and ratios. Moreover, the use of the same surveillance methodology and the same electronic platform ensured the homogeneity of the calculated rates and ratios. Yet, several challenges still need to be overcome to further improve CAUTI surveillance in MOH hospitals, including data validation, site audits and rapid turnover of ICPs (29).
Conclusion
The current study estimated CAUTI rates and UCU ratios in 15 different types of ICUs from 99 MOH hospitals distributed in 20 different regions. The overall CAUTI rate was 1.68 per 1,000 urinary catheter days, and the overall UCU ratio was 0.62. MOH CAUTI rates adjusted for the type of ICUs were 16 to 69% lower than recognised benchmarks. Interestingly, the differences in UCU ratios between this study and recognised international benchmarks were minimal. The current study is a unique national CAUTI benchmark that can potentially help in the fight against HAI (28). As HAIs increase morbidity, mortality, length of hospital stay and financial loss, certain initiatives are necessary to prevent and control them (30).
Acknowledgements
The authors thank General Directorate of Infection Prevention and Control (GDIPC), ICPs (Infection Control Practitioners), Regional Coordinators and HESN (Health Electronic Surveillance Network) Team at Ministry of Health (MOH), Riyadh, Kingdom of Saudi Arabia.
Authors’ contributions
Yvonne S. Aldecoa: Data collection and manuscript writing. Adel Alanazi: Drafting the article and data collection. Ghada Bin Saleh: Data Analysis and interpretation. Nasser Alshanbari: Results calculation and compilation. Tabish Humayun: Study design, Manuscript writing and Discussion. Faisal Alsheddi: Data collection and analysis. Aiman El-Saed: Data Analysis, review of final manuscript and final approval of the manuscript to be published. Mohammed Alqahtani: Results and discussion. Khalid H. Alanazi: Final review and critical revision of the article.
Ethical approval
Ethical approval (exempt status) was provided by the Institutional Review Board, King Fahad Medical City, Riyadh.
References
- Feneley RCL, Hopley IB, Wells PNT. Urinary catheters: history, current status, adverse events and research agenda. J Med Eng Technol 2015; 39(8): 459–70. doi: 10.3109/03091902.2015.1085600
- Klevens RM, Edwards JR, Richards CL, Jr., Horan TC, Gaynes RP, Pollock DA, et al. Estimating health care-associated infections and deaths in U.S. hospitals, 2002. Public Health Rep 2007; 122(2): 160–6. doi: 10.1177/003335490712200205
- World Health Organisation. Report on the burden of endemic health care-associated infection worldwide. A systematic review of the literature. 2011. Available from: http://whqlibdoc.who.int/publications/2011/9789241501507_eng.pdf [cited 01 January 2021).
- Alshamrani MM, El-Saed A, Alsaedi A, El Gammal A, Al Nasser W, Nazeer S, et al. Burden of healthcare-associated infections at six tertiary-care hospitals in Saudi Arabia: a point prevalence survey. Infect Contr Hosp Epidemiol 2019; 40(3): 355–7. doi: 10.1017/ice.2018.338
- Rosenthal VD, Bat-Erdene I, Gupta D, Belkebir S, Rajhans P, Zand F, et al. International Nosocomial Infection Control Consortium (INICC) report, data summary of 45 countries for 2012–2017: device-associated module. Am J Infect Control 2020; 48(4): 423–32.
- Moreno CA, Rosenthal VD, Olarte N, Gomez WV, Sussmann O, Agudelo JG, et al. Device-associated infection rate and mortality in intensive care units of 9 Colombian hospitals: findings of the International Nosocomial Infection Control Consortium. Infect Contr Hosp Epidemiol 2006; 27(4): 349–56. doi: 10.1017/ice.2018.338
- Advani SD, Lee RA, Long M, Schmitz M, Camins BC. The impact of 2015 NHSN Catheter-associated Urinary Tract Infection (CAUTI) definition change on Central Line-associated Bloodstream Infection (CLABSI) rates and CLABSI prevention efforts at an Academic Medical Center. Infect Control Hosp Epidemiol 2018; 39(7): 878–80. doi: 10.1017/ice.2018.338
- Fakih MG, Groves C, Bufalino A, Sturm LK, Hendrich AL. Definitional change in NHSN CAUTI was associated with an increase in CLABSI events: Evaluation of a large health system. Infect Contr Hosp Epidemiol 2017; 38(6): 685–9. doi: 10.1017/ice.2017.41
- Cassini A, Plachouras D, Eckmanns T, Abu Sin M, Blank HP, Ducomble T, et al. Burden of six healthcare-associated infections on European Population Health: Estimating incidence-based disability-adjusted life years through a population prevalence-based modelling study. PLoS Med 2016; 13(10): e1002150. doi: 10.1017/ice.2017.41
- Smith DRM, Pouwels KB, Hopkins S, Naylor NR, Smieszek T, Robotham JV. Epidemiology and health-economic burden of urinary-catheter-associated infection in English NHS hospitals: a probabilistic modelling study. J Hosp Infect 2019; 103(1): 44–54. doi: 10.1016/j.jhin.2019.04.010
- Umscheid CA, Mitchell MD, Doshi JA, Agarwal R, Williams K, Brennan PJ. Estimating the proportion of healthcare-associated infections that are reasonably preventable and the related mortality and costs. Infect Contr Hosp Epidemiol 2011; 32(2): 101–14. doi: 10.1016/j.jhin.2019.04.010
- Ferguson A. Implementing a CAUTI prevention program in an acute care hospital setting. Urol Nurs 2018; 38(6): 273–302. doi: 10.7257/1053-816X.2018.38.6.273
- Van Mourik MSM, Perencevich EN, Gastmeier P, Bonten MJM. Designing surveillance of healthcare-associated infections in the era of automation and reporting mandates. Clin Infect Dis 2018; 66(6): 970–6. doi: 10.1093/cid/cix835
- Menegueti MG, Ciol MA, Bellissimo-Rodrigues F, Auxiliadora-Martins M, Gaspar GG, Canini S, et al. Long-term prevention of catheter-associated urinary tract infections among critically ill patients through the implementation of an educational program and a daily checklist for maintenance of indwelling urinary catheters: a quasi-experimental study. Medicine (Baltimore) 2019; 98(8): e14417. doi: 10.1093/cid/cix835
- Marigliano A, Barbadoro P, Pennacchietti L, D’Errico MM, Prospero E. Active training and surveillance: 2 good friends to reduce urinary catheterization rate. Am J Infect Contr 2012; 40(8): 692–5. doi: 10.1016/j.ajic.2012.01.021
- Palumbo AJ, Loveless PA, Moll ME, Ostroff S. Evaluation of healthcare-associated infection surveillance in Pennsylvania hospitals. Infect Contr Hosp Epidemiol 2012; 33(2): 105–11. doi: 10.1086/663709
- Gaid E, Assiri A, McNabb S, Banjar W. Device-associated nosocomial infection in general hospitals, Kingdom of Saudi Arabia, 2013–2016. J Epidemiol Glob Health 2018; 7(Suppl 1): S35–40. doi: 10.1016/j.jegh.2017.10.008
- Al Nasser W, El-Saed A, Al-Jardani A, Althaqafi A, Alansari H, Alsalman J, et al. Rates of catheter-associated urinary tract infection in tertiary care hospitals in 3 Arabian Gulf countries: a 6-year surveillance study. Am J Infect Contr 2016; 44(12): 1589–94. doi: 10.1016/j.ajic.2016.06.030. PMID: 27692786.
- Al-Tawfiq JA, Amalraj A, Memish ZA. Reduction and surveillance of device-associated infections in adult intensive care units at a Saudi Arabian hospital, 2004–2011. Int J Infect Dis 2013; 17(12): e1207–11. doi: 10.1016/j.ijid.2013.06.015
- Khan ID, Basu A, Kiran S, Trivedi S, Pandit P, Chattoraj A. Device-associated healthcare-associated infections (DA-HAI) and the caveat of multiresistance in a multidisciplinary intensive care unit. Med J Armed Forces India 2017; 73(3): 222–31. doi: 10.1016/j.mjafi.2016.10.008
- Saudi Ministry of Health (MOH). Statistical yearbook 1439H (2018 G). 2019. Available from: https://www.moh.gov.sa/en/Ministry/Statistics/book/Documents/book-Statistics.pdf [cited 01 January 2021).
- National Healthcare Safety Network (NHSN). NHSN patient safety component manual. Januray 2018. Available from: http://www.cdc.gov/nhsn/PDFs/pscManual/pcsManual_current.pdf [cited 1 January 2021).
- GCC Centre for Infection Control and Ministry of National Guard Health Affairs. Healthcare-associated infections surveillance manual. 3rd ed. 2018. Available from: http://ngha.med.sa/English/MedicalCities/AlRiyadh/MedicalServices/Documents/3rd_edition_Surveillance_Manual.pdf [cited 1 January 2021].
- Saudi Ministry of Health (MOH). Health electronic surveillance network. 2020. Available from: https://hesn.moh.gov.sa/webportal/ [cited 1 January 2021).
- Dudeck MA, Edwards JR, Allen-Bridson K, Gross C, Malpiedi PJ, Peterson KD, et al. National Healthcare Safety Network report, data summary for 2013, Device-associated Module. Am J Infect Control 2015; 43(3): 206–21. doi: 10.1016/j.ijid.2013.06.015
- Dudeck MA, Weiner LM, Allen-Bridson K, Malpiedi PJ, Peterson KD, Pollock DA, et al. National Healthcare Safety Network (NHSN) report, data summary for 2012, device-associated module. Am J Infect Contr 2013; 41(12): 1148–66. doi: 10.1016/j.ijid.2013.06.015
- Rosenthal VD, Maki DG, Mehta Y, Leblebicioglu H, Memish ZA, Al-Mousa HH, et al. International Nosocomial Infection Control Consortiu (INICC) report, data summary of 43 countries for 2007–2012. Device-associated module. Am J Infect Contr 2014; 42(9): 942–56.
- El-Saed A, Balkhy HH, Weber DJ. Benchmarking local healthcare-associated infections: available benchmarks and interpretation challenges. J Infect Public Health 2013; 6(5): 323–30. doi: 10.1016/j.ijid.2013.06.015
- Humayun T, Alshanbari N, Alanazi A, Aldecoa YS, Alanazi KH, Saleh GB, et al. Rates of ventilator associated pneumonia in Saudi Ministry of Health Hospitals; a two-year multi-center study. Am J Infect Dis Microbiol. 2021; 9(1): 25–31. doi: 10.12691/ajidm-9-1-6
- Humayun T, Qureshi A, Roweily SF, Carig J, Humayun F. Efficacy of hydrogen peroxide fumigation in improving disinfection of hospital rooms and reducing the number of microorganisms. J Ayub Med Coll Abbottabad 2019; 31(4 Suppl 1): 646–50.