REVIEW ARTICLE
Hand hygiene practices in extreme resource limited situations: an integrative review of the literature
Peta-Anne Zimmerman1,2,3,4, Jocelyne M Basseal5, Sophie Dennis6 and Sharon Salmon7
1 School of Nursing and Midwifery, Griffith University, QLD, Australia; 2 Menzies Health Institute Queensland, Griffith University, QLD, Australia; 3 Gold Coast Hospital and Health Service, QLD, Australia; 4 Collaborative for the Advancement of Infection Prevention and Control, QLD, Australia; 5 Sydney Infectious Diseases Institute, University of Sydney, NSW, Australia; 6 Bristol Medical School, University of Bristol, UK; 7 UNSW Medicine, University of New South Wales, NSW Australia
Abstract
As the COVID-19 pandemic affects more than one hundred million people, worldwide prevention measures, particularly hand hygiene (HH), are crucial to control and limit spread of disease. Yet access to clean water and soap or hand sanitiser may be scarce or unattainable in some situations. This integrative review, based on the framework of Whittemore and Knafl and the quality assessment performed in-line with the Mixed Methods Assessment Tool, aims to identify alternative HH agents and water sources that have demonstrated some efficacy in extreme resource limited situations. Four articles met inclusion criteria, with agents that create friction and repurposed water identified as alternatives to soap and water or hand sanitiser, resulting in reduced microbial load. Sand combined with repurposed cooking water, for example, can be used as an alternate HH measure in extreme resource limitations. Long term effects on skin integrity, compliance, and sustainability of these strategies must be considered.
Keywords: Hand hygiene, hand disinfection, hand washing, infection control, hand sanitiser, health resources
Citation: Int J Infect Control 2022, 18: 21586 – http://dx.doi.org/10.3396/ijic.v18.21586
Copyright: © 2022 Peta-Anne Zimmerman et al. This is an Open Access article distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for any purpose, even commercially, provided the original work is properly cited and states its license.
Received: 4 May 2021; Revised: 23 July 2021; Accepted: 6 September 2021; Published: 30 August 2022
Competing interests and funding: No authors identify any conflict of interest in the production of this paper or in the study.
Peta-Anne Zimmerman, School of Nursing and Midwifery Griffith University, 2.43 G16, Parklands Drive, Southport, QLD, 4215, Australia. E-mail: p.zimmerman@griffith.edu.au, Ph: +61755528780
Communities are frequently faced with a lack of resources to perform traditional hand hygiene (HH). As such alternative options must be identified. This review provides best available evidence of alternative materials for performing HH. Alternative materials for HH can be effectively used until appropriate water, sanitation and hygiene (WASH) alternatives are available.
Background
On 30 January 2020, the World Health Organization (WHO) announced that the COVID-19 outbreak was a Public Health Emergency of International Concern (PHEIC). Initially, most cases were reported from China and those with travel history to China, however to date, this is no longer the case. COVID-19 is an acute respiratory illness caused by a novel human coronavirus (SARS-CoV-2) which causes higher mortality in people aged ≥60 years and those with underlying medical conditions such as cardiovascular disease, chronic respiratory disease, diabetes, and cancer. Prevention and control of infection transmission in the community is therefore imperative (1).
The principles of infection prevention and control (IPC) are the same in all situations, however implementation is dependent on context and resource availability (2). IPC practices are not limited to only healthcare settings; IPC practices are equally important for prevention of infection within the community and need to be practised by the general public. Practising effective HH is one of the key strategies to prevent disease transmission in any setting (3). Hand hygiene practice in its simplest form refers to any action of hand cleansing, but more traditionally includes the use of water and soap, or alcohol-based hand rub (ABHR) (3).
The WHO recently released interim guidelines to assist Member States to improve compliance of HH to prevent the transmission of COVID-19 in the community by: “Providing universal access to public HH stations and making their use obligatory on entering and leaving any public or private commercial building and any public transport facility.” (1) In most situations this is achievable yet these principles and practices do, however, cause an impost on available resources and rely on basic infrastructure and a reliable supply chain. This becomes an issue not only in the current COVID-19 situation but also for future outbreaks and pandemics.
In 2017, WHO and UNICEF reported that 71% of the world’s population has access to safe water sources (4). In extreme resource limited settings where there may be no water and soap or ABHR to perform HH, how can these communities practice HH?
Aim
The aim of this integrative review is to identify HH agents that have shown some efficacy, and could be used as an alternative to, soap and water or ABHR in extreme resource limited situations that have resulted in an absence of normal HH materials.
Method
An integrative review methodology was used as it includes various perspectives on a subject or topic and is currently the broadest type of research review which has been advocated as important to health science and research (5). The framework developed by Whittemore and Knafl (5) guided this review and includes: problem identification, literature search, data evaluation, data analysis, and presentation of the data. The ability to include both experimental and non-experimental research and the use of quality scores to evaluate the overall quality of studies allows for a comprehensive understanding of the topic and a more detailed evaluation of the strategies to implement IPC practices in extreme resource limited contexts (5). To assist in structuring a clinical question, the Population, Intervention, Comparison, Outcome and Context (PICOC) framework was used as it is regarded as a valuable tool to assist with developing evidenced-based medicine (6).
Population: humans
Intervention: alternative HH strategies/agents
Comparison: ABHR, water, soap and water
Outcome: bioburden reduction on hands using alternative HH strategies/agents
Context: resource limitations
Search methods
An electronic database search was conducted including a search of Cumulative Index for Nursing and Allied Health Literature (CINAHL), Embase, and National Library of Medicine (Medline) and included peer reviewed, published literature with no age, human, language limit or geographical restrictions. This search was performed up to and including June 2020. The search terms used included the following MeSH, keywords and Boolean terms of “hand hygiene” OR “hand washing” OR “handwashing” OR “hand rubbing” OR “handrub*” OR “hand disinfection” OR “hand wash” OR “handwash” OR “hand cleaning” OR “hand decontamination” AND “bacteria” OR “virus*” OR “disease” OR “infect*” OR “communicable disease” AND “chlorine” OR “hypochlorite” OR “ash” OR “mud” OR “sand” OR “rice” OR “seawater” OR “dirt” NOT “water supply” OR “water purification” OR “waste water” OR “drinking water”. These search terms represented the most commonly accepted and utilised terminology related to HH practices as reported in the literature. As this study specifically worked to identify non-traditional hand cleansing agents, traditional agents such as soap and ABHR were not sought in this study. Only primary research was included with literature review articles excluded due to risk of missing key pieces based on those reviews specific search strategies.
Articles were screened based on title and abstract with the further review conducted on articles that met the inclusion criteria, by the first author. Reference lists of the selected articles were reviewed to allow for the inclusion of additional articles that may not have initially been identified from the database search. Only literature that met the inclusion criteria was included in the review which were: 1) all alternative HH agents to soap, water, and ABHR, 2) relevant to humans, 3) in vivo experiments and, 4) published in peer-review journals. Exclusion criteria included: 1) studies using soap and water or ABHR, 2) animal studies, 3) in-vitro studies, 4) environmental studies and, 5) studies related to therapy. Included studies were considered to provide valid information in addressing the initial aim of the review to identify alternative strategies for HH in the absence of traditional HH materials or resources.
The initial search identified a total of 125 titles in which one was excluded due to duplication (Figure 1). After an initial screening of the 124 titles and abstracts, a total of 107 articles were excluded as they did not relate specifically to alternative strategies/agents for HH. Of the 17 articles remaining, a further 13 were excluded due to not meeting the inclusion criteria. When required, clarification of article inclusions was made with the second author. A total of four articles were included in the final review that specifically related to the use of alternative HH agents in the absence of traditional HH materials such as soap or ABHR. A systematic flow diagram (Figure 1), based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) was used to display the search strategy and provides a breakdown of the search results (7).
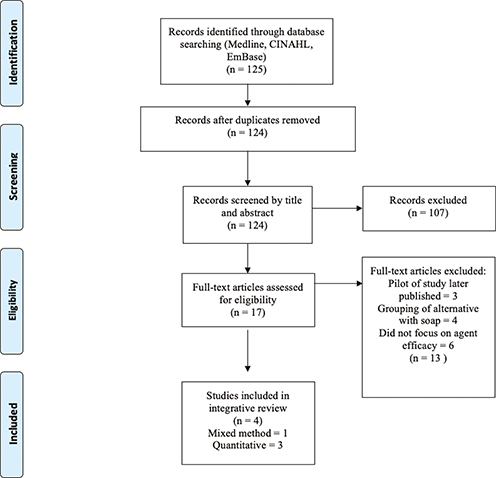
Fig. 1. Article selection flowchart (adapted from Moher et al.7)
Data extraction and synthesis
Articles were reviewed, and information was included on the study method, aim, sample size, HH agent(s) investigated, and overall results. Data extraction was conducted by the first author and reviewed by the second author. The findings from each study were then compared and contrasted to identify themes, similarities or discrepancies to allow for specific themes to be developed from the articles. Analysis of the data resulted in the development of one primary category of note: the use of friction with an abrasive agent.
In order to assess the quality of the articles included in the review the Mixed Methods Appraisal Tool (MMAT) version 2018 was used as it, unlike other appraisal tools, allows for a variety of studies to be included in its assessment including quantitative, qualitative, and mixed methods research designs (8). The MMAT has been reported to have reliability and efficiency with interrater reliability scores ranging from moderate to perfect agreement (8). The MMAT utilises a set of five categories, each with five associated specific criteria, including a qualitative set, a randomised set, a non-randomised set, an observational descriptive set, and a mixed method set. The MMAT version 2018 does not recommend scoring against the category criteria, rather a description of what was met or not met (8). The included studies were appraised independently by the first and second authors, with discrepancies adjudicated by the third author, based on the MMAT version 2018 criteria with no studies excluded based on the quality assessment. Results of the critical appraisal of the papers using the MMAT version 2018 ranged from papers meeting between three and five (out of five) of the criteria.
Results
Four articles met inclusion criteria for the final review, three quantitative and one mixed method study. All included articles were published between 1985 and 2015, with two of the articles published within the last seven years. One of the studies was from a low-income setting, with other studies from the USA and Germany exploring novel strategies for HH in the absence of traditional materials. All studies focused specifically on the use of alternative HH agents that are available in the environment such as sand, soil, ash, or other abrasives that may be found in local stores with small amounts of water and the effect of microbial load on hands. Overall strategies identified from the four articles in the final review included abrasive agents that create friction as alternatives to traditional soap and water, or ABHR, as HH agents. All studies reported reduction of microbial load using the abrasive agent with little water (Table 1). In all studies, small amounts of water were required with each of the agents, followed by rinsing. In one study from Bangladesh, the quality of the water used was variable and often repurposed from other uses such as laundry or dish washing, or using pond water (9). The studies from the USA and Germany utilised available running water from municipal water sources (10–12). Importantly, there were no published studies that investigated HH in the complete absence of water or other forms of wetting agents.
| Reference | Study design/method | Sample size | Aim | Population | Hand hygiene (HH) agent | Results | Limitations/MMAT (2018)(8) |
| Schurmann et al. (12) (1985) Germany | Quantitative in vivo experimental | Three | Establish efficacy of HH agents to remove poliovirus from hands | Polio immunised participants | -Sand/water -Soap/water -Aluminium hydroxide powder/water |
Washing agents more effective than soap & water were: sand log10 reduction 3.7 and aluminium hydroxide powder log10 reduction 3.2, compared to soap and water log10 reduction 1.9, suggesting that friction was more important than emulsification. |
Large numbers of virus particles used, perhaps not real-life contamination/All quality criteria met for quantitative studies |
| Hoque et al. (1995) Bangladesh (9) | Mixed methods -Observation of practice -Measurement of faecal coliforms on hands |
90 participants | Understanding effect of HH practices on faecal coliform counts | Women semi-rural |
-Soil/water -Soap/water -Ash/water -Water only |
Lower coliform counts with increased rubbing frequency. Increased volumes of rinse water lowers coliform counts, dependent on water quality. All agents showed comparable results. |
Compared left with right hands, no average coliform count over both/Criteria 5.3 and 5.5 for mixed methods studies not met |
| Edmonds et al. (2013) USA (10) | Quantitative experimental | nine | To compare the efficacy of various hand washing preparations at removing C. difficile. | Experiment participants | -Soap/water -Various soaps/waters -Sodium tetraborate decahydrate powder/water -Ink & stain remover/water -Ink & stain remover + brush/water |
BoraxTM log10 reduction 1.18 (P<.05), ink & stain remover log10 reduction 1.21(P<.001), ink & stain remover + brush log10 reduction 1.47 (P<.0001), water log10 reduction 0.76, with soap and water log10 reduction 0.78 (P>.05). | Number of samples tested for each agent was not uniform/All quality criteria met for quantitative studies |
| Isaacson et al. (2015) USA (11) | Quantitative experimental | 14 participants | Measure efficacy of five HH agents against Clostridium difficile | Healthcare workers | -Water rub/rinse -Triclosan soap/water -Sand/water -Oil/baking powder/dish detergent/water -60-second water rinse |
Sand/water had greatest average log difference compared with water rub/rinse (P=.019) and triclosan soap/water (P=.003) Friction important for removal of spores. |
Triclosan not sporicidal. Only tested against spore forming organism/All quality criteria met for quantitative studies |
The use of friction for hand hygiene
In the four studies identified from this review alternative HH agents to soap and water and ABHR included the use of either: 1) ash (9), 2) soil (9), 3) sand (11,12), 4) oil/baking powder/dish detergent (11), 5) aluminium hydroxide powder (10), 6) sodium tetraborate decahydrate powder (BoraxTM) (10), 7) ink and stain remover +/- brush (10), or 8) water only (9–12), and compared these with a soap and water strategy (9,11). The most successful agents used in these studies were physically abrasive and were of a powder or grit consistency, or in the case of the study by Edmonds and colleagues (10), actively used a brush to create friction with an ink and stain remover agent. All the agents created friction with use of a wetting agent such as water to decontaminate hands and were found to be superior to using soap and water or only water in some cases based on the testing methods reported in the papers, which were not standardised across all studies. Table 2 indicates reduction of microbial load count using friction only.
| Study | Sand | Ash | Soil | Oil/baking powder/detergent | Aluminium hydroxide powder | Sodium tetraborate decahydrate powder | Ink & stain remover + brush | Water | Soap & water |
| Schurmann et al. (12) | Log10 3.7 reduction | NA | NA | NA | Log10 3.2 reduction | NA | NA | NA | Log10 1.9 reduction |
| Hoque et al. (9) | NA | 98 cfu | 129 cfu | NA | NA | NA | NA | 288 cfu | 195 cfu |
| Edmonds et al. (10) | NA | NA | NA | NA | NA | Log10 1.18 reduction (P<.05) |
Log10 1.47 reduction (P<.0001) |
Log10 0.76 reduction | Log10 0.78 reduction (P>.05) |
| Isaacson et al. (11) | -0.50 average log difference (to soap and water) (P=.003) |
NA | NA | -0.37 average log difference (to soap and water) (P=.001) |
NA | NA | NA | -0.14 average log difference (to soap and water) (P=.246) |
comparator |
Discussion
This integrative review demonstrates that whilst there is a paucity of literature available that provides evidence on HH agents that may be readily accessible in resource limited settings, those studies that are available demonstrate that an agent that creates friction to clean the hands, using a lubricating agent such as water, is arguably effective to perform HH in the absence of soap and clean water (9–12). This has been supported elsewhere indicating the action of creating friction for at least 20 seconds even with water alone decreases the biological burden of contaminated hands (13).
What these studies were not able to identify however is the sustainability of these agents from a compliance perspective and what the effect may be of their long-term use, such as dermatitis which could lead to infection due to poor skin integrity and wounds. Other studies have identified that the more caustic or abrasive a HH agent is such as chlorine or other chemicals, the less likelihood there is of sustained adoption of practices (3, 14–16).
All the studies presented required the use of water to complete the HH practice and were more often than not used as a lubricant with the agent to provide the friction to clean and also rinse the hands. Given that 71% of the global population has access to improved safe water sources, this appears to be a reasonable strategy (4). Even so, three of the studies were conducted using municipal water (10–12), with one using repurposed waste or pond water with an unknown bioburden (9). Interestingly, the use of potentially contaminated water in conjunction with the friction generating HH agent still reduced the number of colony forming units on the hands of participants (9), which has also been reported elsewhere (17–22). This then begs the question as to how other sources of water could be repurposed for use for HH, such as seawater, as has been proposed in a study to create a 0.05% hypochlorite solution for HH using sodium chloride-based water (23). The health outcomes of using alternative water sources were not reported. This is an important consideration as the use of contaminated water, particularly with coliforms, can result in outbreaks of diarrhoeal disease with poor individual and community health outcomes (4). Where clean water is lacking in limited resource environments, it is therefore possible to consider alternate water sources, the cleaner the better, to be used in HH practices.
In an effort to address these issues and specific requests for advice, the World Health Organization Regional Office for the Western Pacific (WPRO) sought to provide advice to their member states on how to achieve HH in the absence of traditional materials such as clean water, soap, or ABHR. This resulted in the production and dissemination of “Considerations for community HH practices in low-resource situations,” (24) and the associated visual resource “Handwashing in low resource settings.” (25). The visual material has now been translated into five languages (Khmer, Laos, Bahasa Melayu, Samoan, and Papa New Guinean) and used in communities where access to traditional HH materials is problematic, such as Papua New Guinea.
Another important aspect of HH not included in any of these articles was the drying of hands after cleaning. Drying of hands is an important part of the HH process as moisture on hands can contribute to transmission of organisms. This has been demonstrated in a community based study where transmission of organisms was reduced by up to 99.8% if hands were dried effectively after cleaning (26). This now introduces the next question: how can hands be dried effectively with limited resources?
A limitation of this review is a clear lack of available literature that investigates the use of HH resources alternative to traditional materials, identifying the need for further research, preferably in the field of how HH practice can be adapted to extreme resource limitations, and prevent transmission of communicable disease in vulnerable communities.
Conclusion
Supporting and implementing HH practices in the community, regardless of resource availability, is crucial in the prevention and control of communicable diseases, and particularly important given increasing emerging and re-emerging pathogens. The principles of HH, like all IPC practices, are always the same; it is how we apply them to specific situations and contexts using available resources that is essential to successful and sustainable implementation. The use of sand as a friction generating agent in conjunction with water from a source that is as clean as possible, based on the available limited evidence, demonstrates efficacy against soap and water. There is, however, no evidence of the sustainability of this strategy to clean hands or what the long-term effect is on skin integrity.
Engaging with communities to identify and promote local methods to perform HH is required, including the recognition of alternative safe water sources and traditional agents/indigenous flora such as leaves, roots, and other friction generating substances in the environment.
Acknowledgements
The authors wish to acknowledge the untiring work of WPRO who produced the regional guidance (24) and visual aid (25) based on this review of the literature, particularly the Infection Prevention and Control and Risk Communication and Community Engagement teams with special thanks to Mr Antonio Perez, the designer and illustrator of the visual aid.
Ethics and consent
Not applicable.
References
| 1. | World Health Organization. Recommendations to Member States to improve hand hygiene practices to help prevent the transmission of the COVID-19 virus: Interim Guidance April 1 2020. Geneva: World Health Organization; 2020. https://www.who.int/publications/i/item/recommendations-to-member-states-to-improve-hand-hygiene-practices-to-help-prevent-the-transmission-of-the-covid-19-virus [Accessed 21 July, 2021]. |
| 2. | World Health Organization. Responding to community spread of COVID-19: Interim guidance 7 March 2020. Geneva: World Health Organization; 2020. https://apps.who.int/iris/handle/10665/331421 [Accessed 21 July, 2021]. |
| 3. | Pittet D, Allegranzi B, Boyce J. The World Health Organization guidelines on hand hygiene in health care and their consensus recommendations. Infect Control Hosp Epidemiol 2009; 30: 611–622. |
| 4. | World Health Organization, UNICEF. Progress on drinking water, sanitation, and hygiene, 2000–2017. Special focus on inequalities. New York: United Nations Children’s Fund and World Health Organization; 2019. https://data.unicef.org/resources/progress-drinking-water-sanitation-hygiene-2019/ [Accessed 21 July, 2021]. |
| 5. | Whittemore R, Knafl K. The integrative review: updated methodology. J Adv Nurs 2005; 52: 546–553. |
| 6. | Huang X, Lin J, Demner-Fushman D. Evaluation of PICO as a knowledge representation for clinical questions. AMIA Ann Symp Proc 2006; 359–363. |
| 7. | Moher D, Liberati A, Tetzlaff J, Altman DG, for the PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009; 6: 338:b2535. |
| 8. | Hong QN, P P, Fabregegues S, et al. Mixed Methods Appraisal Tool (MMAT) version 2018. Registration of Copyright (#1148552) ed. Canada: Canadian Intellectual Property Office, Industry Canada.; 2018. |
| 9. | Hoque BA, Mahalanabis D, Alam MJ, Islam MS. Post-defecation handwashing in Bangladesh: practice and efficiency perspectives. Public Health 1995; 109: 15–24. |
| 10. | Edmonds SL, Zapka C, Kasper D, et al. Effectiveness of hand hygiene for removal of Clostridium difficile spores from hands. Infect Control Hosp Epidemiol 2013; 34: 302–305. |
| 11. | Isaacson D, Haller B, Leslie H, Roemer M, Winston L. Novel handwashes are superior to soap and water in removal of Clostridium difficile spores from the hands. Am J Infect Control 2015; 43: 530–532. |
| 12. | Schürmann W, Eggers HJ. An experimental study on the epidemiology of enteroviruses: water and soap washing of poliovirus 1--contaminated hands, its effectiveness and kinetics. Med Microbiol Immunol 1985; 174: 221–236. |
| 13. | Miller T, Patrick D, Ormrod D. Hand decontamination: influence of common variables on hand-washing efficiency. Healthc Infect 2011; 16: 18–23. |
| 14. | Tuck JJH, Williams JR, Doyle AL. Gastro Enteritis in a military population deployed in West Africa in the UK Ebola response; was the observed lower disease burden due to handwashing? Travel Med Infect Dis 2016; 14: 131–136. |
| 15. | Wolfe MK, Gallandat K, Daniels K, Desmarais AM, Scheinman P, Lantagne D. Handwashing and Ebola virus disease outbreaks: A randomized comparison of soap, hand sanitizer, and 0.05% chlorine solutions on the inactivation and removal of model organisms Phi6 and E. coli from hands and persistence in rinse water. PloS ONE 2017; 12: e0172734. |
| 16. | Wolfe MK, Wells E, Mitro B, Desmarais AM, Scheinman P, Lantagne D. Seeking Clearer Recommendations for Hand Hygiene in Communities Facing Ebola: A Randomized Trial Investigating the Impact of Six Handwashing Methods on Skin Irritation and Dermatitis. PloS ONE 2016; 11: e0167378. |
| 17. | Baker KK, O’Reilly CE, Levine MM, et al. Sanitation and Hygiene-Specific Risk Factors for Moderate-to-Severe Diarrhea in Young Children in the Global Enteric Multicenter Study, 2007–2011: Case-Control Study. PLoS Med 2016; 13: 1–19. |
| 18. | Edward A, Jung Y, Chhorvann C, Ghee AE, Chege J. Association of mother’s handwashing practices and pediatric diarrhea: evidence from a multi-country study on community oriented interventions. J Prev Med Hyg 2019; 60: E93–E102. |
| 19. | Huda TMN, Unicomb L, Johnston RB, Halder AK, Yushuf Sharker MA, Luby SP. Interim evaluation of a large scale sanitation, hygiene and water improvement programme on childhood diarrhea and respiratory disease in rural Bangladesh. Soc Sci Med 2012; 75: 604–611. |
| 20. | Lohiniva AL, Saeed M, El-Sayeed N, Talaat M. Clean hands: prevention of typhoid fever in rural communities in Egypt. Int Q Community Health Educ 2007; 28: 215–227. |
| 21. | Ravindra K, Mor S, Pinnaka VL. Water uses, treatment, and sanitation practices in rural areas of Chandigarh and its relation with waterborne diseases. Environ Sci Poll Res Int 2019; 26: 19512–19522. |
| 22. | Ray SK, Dobe M, Lahiri A, Basu SS. Hand washing practices in urban and rural communities in and around Kolkata, West Bengal. Indian J Public Health 2009; 53: 192–195. |
| 23. | Hitomi S, Baba S, Yano H, Morisawa Y, Kimura S. Antimicrobial effects of electrolytic products of sodium chloride--comparative evaluation with sodium hypochlorite solution and efficacy in handwashing. Kansenshogaku Zasshi 1998; 72: 1176–1181. |
| 24. | World Health Organization. Regional Office for the Western Pacific. Considerations for community hand hygiene practices in low-resource situations. Manila: WHO Regional Office for the Western Pacific; 2020. https://apps.who.int/iris/handle/10665/332382 [Accessed 21 July, 2021]. |
| 25. | World Health Organization Regional Office for the Western Pacific. Handwashing in low resource settings. Manila: WHO Regional Office for the Western Pacific; 2020. https://www.who.int/westernpacific/internal-publications-detail/handwashing-in-low-resource-settings [Accessed 21 July, 2021]. |
| 26. | Patrick D, Miller TE, D O. Reduction of microbial transmission in childcare using an improved hand drying protocol. Healthc Infect 2010; 15: 15–19. |