ORIGINAL ARTICLE
Hand hygiene knowledge, attitudes, and self-reported practices among medical and nursing staff of a tertiary-care military hospital: a cross-sectional study
Iqra Zia*, Sidra Shafiq Cheema, Naveen Siddique Sheikh and Huma Ashraf
Combined Military Hospital, Lahore, Pakistan
Abstract
Hand hygiene (HH) serves as a primary public health measure against healthcare-associated infections. During the coronavirus disease 2019 (COVID-19) pandemic, caused by the severe acute respiratory syndrome (SARS) coronavirus 2 (SARS-CoV-2), HH has been fundamentally reinforced for preventing infection transmission globally. This cross-sectional study provides data as a baseline evaluation of knowledge, attitude, and self-reported practice, along with the differences of each between medical and nursing staff. A self-administered questionnaire comprising a standardized World Health Organization Hand Hygiene Knowledge Questionnaire (WHO, revised August 2009) and Likert scales for attitude and practice was employed, using convenience sampling to collect data from 383 healthcare workers (HCWs), 92 nurses (24.9%), and 277 doctors (75.1%) in a tertiary-care military hospital. Both nurses and doctors had moderate knowledge with no significant difference (P = 0.54). Moreover, attitude and practice were reported as moderate for both groups. However, the self-reported HH practice of doctors was significantly (P < 0.05) better than that of nurses, while nurses had significantly better (P < 0.01) attitudes in comparison with doctors. Participants who had received formal training in the previous 3 years were 70.65% among nurses and 44.76% among doctors. In total, 78.36% acknowledged routine use of alcohol-based hand rub. It suggested a relationship of HH to demographic variables, professional role, and departmental service. It should be noted that this study shows no relationship between knowledge and practice, and a negative correlation between knowledge and attitude. Concurrently, while further investigation is required to pinpoint the obstacles to achieving proper HH, it can be concluded that infrastructure promoting its practice among HCWs needs to be established.
Keywords: hand hygiene; COVID-19; healthcare workers; knowledge; attitudes; survey; Pakistan
Citation: Int J Infect Control 2022, 18: 21469 – http://dx.doi.org/10.3396/ijic.v18.21469
Copyright: © 2022 Iqra Zia et al. This is an Open Access article distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for any purpose, even commercially, provided the original work is properly cited and states its license.
Received: 24 March 2021; Accepted: 30 September 2021; Published: 12 May 2022
Competing interests and funding: The authors report no conflict of interest. No funding was received for this study.
*Iqra Zia, CMH Lahore Medical College, IOD Abdur Rehman Road, Lahore Cantt 54810, Pakistan. Email: iqrazia.ak@outlook.com
Hands of healthcare workers (HCWs) become routinely colonized during patient care, serving as vehicles for transmission and leading to healthcare-associated infection (HCAI) (1, 2). HCAI occurs during the process of care in a hospital or another healthcare facility, with the infection not having been present or incubating at the time of admission (3). In a healthcare facility, the sources of infection, and of the preceding contamination, may be personnel, patients, or the inanimate environment, transmitted mostly via large droplets and direct contact with infectious materials (4). HCAI can be prevented by proper HH, which refers to any act of hygienic hand antisepsis to reduce transient microbial flora (2).
The coronavirus disease 2019 (COVID-19) pandemic, caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has put forth HH practices for preventing infection transmission. Together with research into effective treatment and immunization against SARS-CoV-2, further studies of HH practices and behavior remain crucial. While the incidence of HCAI in developed countries varies between 5.1 and 11.6%, rates in developing countries (up to 19%) are markedly higher (3). Ranked as one of the top 10 causes of hospital-related deaths, its implications include prolonged hospital stays, long-term disability, cross-transmission of antimicrobial-resistant pathogens, and financial burden (3). Despite its importance for patient and staff safety, HCW compliance with HH remains poor, being a major public health concern (5, 6). Together with diagnostic difficulties, lack of surveillance systems, and the implementation of basic infection control measures, HCAI greatly overwhelms the capacity of economically constrained developing countries. Notable factors impacting compliance with HH are inadequate knowledge, poor attitude, scarcity of resources, lack of role models, high workload and behavioral perceptions, lack of training and feedback, male gender, lack of time, and understaffing (6–11). Furthermore, studies conducted on HCWs reported moderate knowledge (9, 12). However, studies showed low attitude toward HH and a significant relationship between improved practices and formal training and education (13, 14).
In Pakistan, with economic constraints, inadequate infection-control practices, lack of proper surveillance programs, and inequities in the healthcare system, there is a paucity of data exploring this subject. However, one study signified better HH knowledge among physicians as compared with the nursing group (63.1%); however, there was no significant difference in the practice of HH in compliance with recommended HH guidelines (15). Another study conducted in Karachi demonstrated 12.3% compliance among HCWs, with 62.73% of participants being aware of the World Health Organization (WHO) guidelines on HH. Despite 65.56% of participants being aware of HCAI, more than half of the participants (62.26%) were unaware of their complications including life-threatening infections, especially among immunocompromised patients, and 45.75% had never attended a formal lecture on the subject (11).
In the interests of improving the quality of healthcare services through adherence to hand hygiene (HH) standards and precautions that need to be promoted through structured training and surveillance programs, this study aimed to provide baseline data regarding knowledge, attitude, and self-reported practice among healthcare workers (HCWs); assess and identify gaps and factors affecting knowledge, attitude, and practice among HCWs; and evaluate the difference between medical and nursing staff knowledge, attitude, and practice of HH.
Methods
A cross-sectional study was conducted using convenience sampling technique on eligible medical and nursing staff, working in a tertiary military hospital of Lahore, Pakistan. Data were collected from September 2019 to August 2020. The minimum sample size required was 370 using the WHO sample calculator at a 95% confidence interval and 5% precision with the assumption of a 60% noncompliance rate. To reduce bias, a self-administered questionnaire of standardized scales was built comprising four parts, namely, demographics, WHO Hand Hygiene Knowledge Questionnaire (16), and two scales adopted from a previous study to assess attitude and practice (17). Participants were aware of the voluntary nature of this study and provided their informed consent before completing the questionnaire.
Instruments
WHO Hand Hygiene Knowledge Questionnaire
The scale is a 21-item tool to assess HH knowledge using questions with yes/no and multiple choice answers regarding the route, source, and prevention of HCAI, along with the best-suited methods of HH in various situations. It includes a short glossary for definitions of terms like hand rubbing, handwashing, etc. for a better understanding of the respondents. Scores above 75% were considered good, 50–74% were considered moderate, and less than 50% were considered poor.
Scales for attitude and practice
Attitude toward HH practice, adherence, importance, and priorities, along with self-reported practices, were assessed using the scales adopted from a previous study (17). Attitude can be defined as a HCW’s perception of the importance of HH and the psychological tendency expressed by evaluating HH with some degree of favor or disfavor. These tools employ a Likert scale with five possible responses ranging from 1 (strongly disagree) to 5 (strongly agree). The attitude toward HH is a 10-item scale, and HH practice is a six-item self-reported scale with each item having a maximum score of 5, making total possible scores of 50 and 30, respectively. Scores higher than 75% were considered good, 50–74% were considered moderate, and less than 50% were considered poor.
Statistical methodology
Data were entered into Statistical Package for Social Sciences (SPSS Statistics for Windows Version 20, IBM Corporation, Armonk NY) for analysis. Data were analyzed using descriptive analysis (means, frequency, percentages, and standard deviation) and inferential analyses (Pearson product-moment coefficient of correlation, chi-square analysis, independent sample t-test, and multiple linear regressions). A P-value of <0.05 was considered statistically significant.
Results
Questionnaires were distributed to 383 participants, four of whom were discarded due to missing responses on attitude and practice measures. A few additional questionnaires were completed but the service, ward, and department were not specified; the ‘other’ category is inclusive of but not limited to these responses. Missing data of remaining participants were under the acceptable range (<10%).
Demographics
The mean age of the 379 participants was 23.25 (standard deviation = 7.45) years, whereby 92 (24.9%) were nurses and 277 (75.1%) were doctors (Table 1).
Knowledge, attitude, and self-reported practice
Responses to the WHO knowledge questionnaire are represented in Table 2. Regarding routine use of alcohol-based hand rub (ABHR), 76.08% (n = 70) of nursing staff agreed; however, among the doctors’ group, it was 81.94% (n = 227). While 70.65% (n = 65) nurses received formal training in the last 3 years, it was 44.76% (n = 124) among doctors.
| No. | Questions (Answers) | Total sample n (%) | Nurses n | Doctors n | P |
| 1 | Which of the following is the main route of cross-transmission of potentially harmful germs between patients in a healthcare facility? (Healthcare workers’ hands when not clean) | 215 (56.72) | 64 | 151 | 0.01** |
| 2 | What is the most frequent source of germs responsible for healthcare-associated infections? (Germs already present on or within the patient) | 62 (16.36) | 28 | 34 | 0.01*** |
| 3 | Which of the following hand hygiene actions prevents transmission of germs to the patient? | ||||
| Immediately after a risk of body fluid exposure (Yes) | 310 (81.79) | 64 | 246 | 0.01** | |
| Before touching a patient (Yes) | 348 (91.82) | 88 | 260 | 0.35* | |
| After exposure to the immediate surroundings of the patient (No) | 53 (13.98) | 16 | 37 | 0.71* | |
| Immediately before a clean/aseptic procedure (Yes) | 299 (78.89) | 58 | 241 | 0.01*** | |
| 4 | Which of the following hand hygiene actions prevents transmission of germs to the healthcare worker? | ||||
| After touching a patient (Yes) | 345 (91.03) | 92 | 253 | 0.01*** | |
| Immediately after a risk of body fluid exposure (Yes) | 329 (86.81) | 81 | 248 | 0.07* | |
| Immediately before a clean/aseptic procedure (No) | 65 (17.15) | 18 | 47 | 0.37* | |
| After exposure to immediate surroundings of the patient (Yes) | 325 (85.75) | 79 | 246 | 0.21* | |
| 5 | Which of the following statements on ABHR and handwashing with soap and water are true? | ||||
| Handwashing and hand rubbing are recommended to be performed in sequence (False) | 204 (53.83) | 58 | 146 | 0.03** | |
| Hand rubbing is more effective against germs handwashing. (False) | 212 (55.94) | 35 | 177 | 0.01*** | |
| Hand rubbing is more rapid for hand cleansing than handwashing (True) | 317 (83.64) | 83 | 234 | 0.12* | |
| Hand rubbing causes skin dryness more than handwashing (False) | 137 (36.15) | 29 | 108 | 0.30* | |
| 6 | What is the minimal time needed for an ABHR to kill most germs on your hands? (20 sec) | 203 (53.56) | 21 | 182 | 0.01*** |
| 7 | Which type of hand hygiene method is required in the following situations? | ||||
| Before palpation of the abdomen (Rubbing) | 268 (70.71) | 79 | 189 | 0.01*** | |
| After removing examination gloves (Washing) | 174 (45.91) | 56 | 118 | 0.01*** | |
| Before giving an injection (Rubbing) | 232 (61.21) | 56 | 176 | 0.47* | |
| After emptying a bedpan (Washing) | 281 (74.14) | 63 | 218 | 0.09* | |
| After making a patient’s bed (Rubbing) | 110 (29.02) | 32 | 78 | 0.21* | |
| After visible exposure to blood (Washing) | 279 (73.61) | 64 | 215 | 0.16* | |
| 8 | Which of the following should be avoided, as associated with an increased likelihood of colonization of hands with harmful germs? | ||||
| Damaged skin (Yes) | 346 (91.29) | 91 | 255 | 0.03** | |
| Regular use of a hand cream (No) | 163 (43.00) | 53 | 110 | 0.01*** | |
| Wearing jewelry (Yes) | 299 (78.89) | 70 | 229 | 0.20* | |
| Artificial fingernails (Yes) | 345 (91.03) | 87 | 258 | 0.60* | |
| Chi square analysis: *nonsignificant; **significant at P < 0.05; ***highly significant at P < 0.01. ABHR: alcohol-based hand rub |
|||||
In the attitude section (Fig. 1), more than 50% of respondents agreed that wearing gloves reduces the need for hand-washing practices, while they reported denial of adherence to correct practice at all times and negated feeling guilty after omitting appropriate practice.
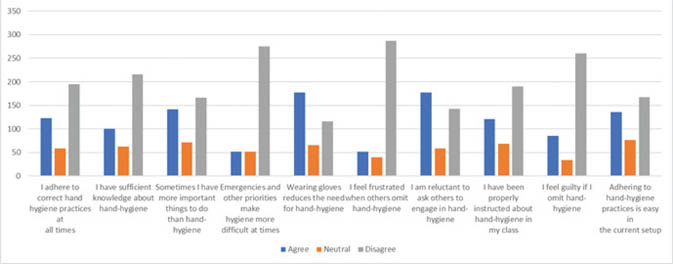
Fig. 1. Attitude toward hand-hygiene among healthcare workers. Vertical (Y) axis represents the number of respondents.
In the practice section (Fig. 2), more than half of the respondents denied recognizing HH as part of their role and also undermined the positive influence of the infection-prevention team.
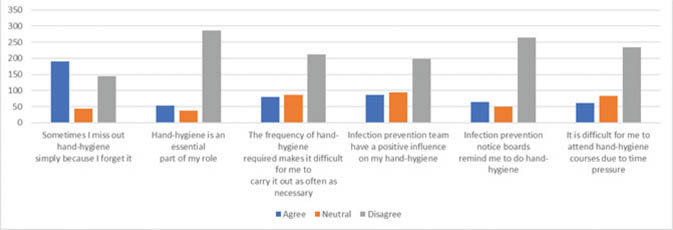
Fig. 2. Practice of hand-hygiene among healthcare workers. Vertical (Y) axis represents the number of respondents.
Comparison of knowledge, attitude, and self-reported practice between nurses and doctors
The categorical analysis of frequency distribution of responses (Table 3) reflects the majority of doctors having the following scores: knowledge 137 (49.5%), attitude 156 (56.4%), and self-reported practice 114 (41.2%). The average scores of nurses include knowledge 39 (42.4%), attitude 46 (50.0%), and self-reported practice 43 (46.8). At P < 0.05, a significant difference in moderate knowledge, self-reported practice, and all categories of attitude was found between nurses and doctors.
| Categories | Nurses n (%) | Doctors n (%) | P |
| Good knowledge | 19 (20.6) | 41 (14.8) | 0.19* |
| Moderate knowledge | 34 (37.0) | 137 (49.5) | 0.04** |
| Poor knowledge | 39 (42.4) | 99 (35.7) | 0.25* |
| Good attitude | 34 (37.0) | 45 (16.2) | 0.001*** |
| Moderate attitude | 46 (50.0) | 76 (27.4) | 0.01*** |
| Poor attitude | 12 (13.0) | 156 (56.4) | 0.01*** |
| Good practice | 13 (14.1) | 66 (23.8) | 0.05** |
| Moderate practice | 36 (39.1) | 97 (35.0) | 0.48* |
| Poor practice | 43 (46.8) | 114 (41.2) | 0.35* |
| Chi-square analysis: *nonsignificant; **significant at P < 0.05; ***significant at P < 0.01. | |||
Further analysis using an independent sample t-test (Table 4) showed that nurses (15.90 ± 2.71) and doctors (16.09 ± 2.45) had moderate knowledge. The mean score of attitudes was interpreted as moderate for both doctors (32.04 ± 5.66) and nurses (36.26 ± 3.64). Furthermore, the mean score for practice was interpreted as moderate for both groups, with doctors having 21.26 ± 3.67 score and nurses having 20.54 ± 2.45 score.
Factors associated with HH knowledge, attitude, and practice
Multiple linear regression of demographics revealed significant predictors of knowledge, attitude, and practice among HCW, as represented in Table 5.
| Variables | B | SE | β | R2 | ΔR2 |
| Knowledge | |||||
| Age | 0.01** | 0.03 | 0.20 | 0.04 | 0.04 |
| Surgery service | −0.86** | 0.33 | −0.14 | 0.07 | 0.06 |
| Mixed medical/surgical service | 1.23** | 0.41 | 0.16 | 0.07 | 0.06 |
| Surgery department | −0.76* | 0.35 | −0.12 | 0.09 | 0.06 |
| Pediatrics department | 1.39** | 0.44 | 0.17 | 0.09 | 0.06 |
| Outpatient clinic department | 5.04* | 2.50 | 0.10 | 0.09 | 0.06 |
| Attitude | |||||
| Gender | −1.61** | 0.58 | −0.14 | 0.02 | 0.01 |
| Gynecology service | −4.39** | 1.10 | −0.20 | 0.12 | 0.11 |
| Pediatrics service | −5.45** | 0.86 | −0.33 | 0.12 | 0.11 |
| Nurse profession | 5.42** | 1.55 | 0.17 | 0.14 | 0.12 |
| Resident profession | −2.03** | 0.75 | −0.14 | 0.14 | 0.12 |
| Nurse student profession | 3.60** | 0.70 | 0.27 | 0.14 | 0.12 |
| Intensive care unit department | 3.00* | 1.12 | 0.13 | 0.18 | 0.16 |
| Obstetrics department | −4.87** | 1.15 | −0.21 | 0.18 | 0.16 |
| Pediatrics department | −5.77** | 0.89 | −0.33 | 0.18 | 0.16 |
| Self-reported practice | |||||
| Mixed medical/surgical service | −1.87** | 0.66 | −0.16 | 0.04 | 0.02 |
| Intensive care ward | −3.02** | 0.73 | −0.22 | 0.06 | 0.04 |
| Multiple linear regression: B, unstandardized regression coefficient; β, standardized regression coefficient; ΔR2, adjusted R2; *P < 0.05, **P < 0.01. | |||||
Correlation of HH knowledge, attitude, and self-reported practice
Table 6 suggests a significant, however ‘very weak’ (r = 0.15) negative correlation between knowledge and attitude with no significant association between knowledge and practice or practice and attitude.
| Variables | 1. Knowledge | 2. Attitude | 3. Self-reported practice |
| 1. Knowledge | - | −0.15** | 0.02 |
| 2. Attitude | - | 0.53 | |
| 3. Self-reported practice | - | ||
| M (SD) | 16.00 (2.59) | 33.20 (5.52) | 21.17 (3.44) |
| Pearson product coefficient correlation: **P < 0.01. | |||
Discussion
HCAI, a major threat to patient safety, can be prevented by appropriate HH practice. In the study, overall, HCWs have moderate knowledge and self-reported practice (Table 3). A satisfying knowledge score is consistent with study at the undergraduate level in Pakistan, whereby both the medical and nursing students demonstrated moderate knowledge (14). A study in India showed good knowledge scores across all professional categories of HCW (18). This observation is reassuring, as a study in Canada identified knowledge as a factor influencing HH compliance (19). However, a study at Stanford University (USA) found that knowledge was not a significant predictor of HH behavior (20). Attitude toward HH is of utmost importance as it is associated with knowledge regarding multidrug-resistant organisms (21), which is an emerging challenge. Training on HH including improvement of knowledge of HH helps in developing a positive attitude toward the prevention of infections by shaping HCW beliefs and perceptions about HH. The study revealed a statistically significant difference between the attitudes of doctors and nurses toward HH, with nurses having better attitudes than doctors (Table 3). The results are comparable with other studies, which reported significantly better attitudes among nurses in comparison with residents (9) and physicians (22).
More than half of the participants (58.2%)—a significant (P = 0.01) fraction of whom were doctors—acknowledged HCWs’ hands as the main vector for cross-transmission between patients. However, the most frequent source of germs was recognized as HCWs’ hands by a low percentage (16.8%) of respondents among which doctors responded proportionately (P < 0.01) better than nurses (Table 2). This finding is comparable with a study in India whereby 45% of residents and 27% of nurses were aware of HCWs’ hands being the most frequent source of germs, with the former having significantly better knowledge (9). While the majority responded correctly in relevance to ‘My 5 Moments of Hand Hygiene’ (2), more than 90% of respondents acknowledged the risk of cross-transmission both ‘before’ and ‘after’ touching patients (Table 2). This is a positive finding as it shows HCW realization of HH for self-protection and patient safety. In contrast, a study in Benin observed more compliance with HH ‘after body fluid exposure’ and ‘after patient contact’ implying a self-protection tendency (23). Supporting this observation, a qualitative study in Canada reported self-protection as the primary reason for performing HH (24). Nevertheless, an overwhelming percentage were unable to correctly identify non-indications, similar to the findings of a Turkish hospital intensive care unit (ICU) (25). It can lead to a waste of time and effort; however, this has been appeased by the finding that the frequency of HH activities was not a barrier to correct practices (Fig. 2).
Despite working in tertiary healthcare with ample opportunities of teaching and training HH, dissatisfaction with the instructions or training provided (50.1%) may attribute to disagreement (>50%) of having sufficient knowledge regarding HH (Fig. 1). This observation is important as studies positively correlate educational intervention and training with improved knowledge (26, 27), self-reported practice, and compliance (13, 26). Almost 70% of the study population denied the relevance and utility of infection-prevention notice boards (Fig. 2), contrary to a study in India supporting their use to reinforce attitude (18). A study in the United States reported a decrease in noncompliance rate from 74.06% at baseline to 36.66% after the introduction of HH posters (28).
The use of ABHR at point of care is preferred for routine HH when hands are not visibly soiled, providing convenience, better skin tolerability, and easy availability along with optimal antimicrobial efficacy. Notably, a major proportion (>50%) admitted its routine use; however, a high percentage of respondents (nearly 60%) wrongly associated hand rubbing with skin dryness (Table 2). By comparison with the doctors, a poor response was observed by nurses regarding situations like ‘before palpation of abdomen’ (P < 0.01) and ‘after removing examination gloves’ (P < 0.01) (Table 2). This finding is imperative as nurses perform the greatest amount of direct patient care and therefore require an optimal level of knowledge regarding precautions, especially related to gloves. Regarding the use of gloves, it has been observed that HH compliance was significantly poor when gloves were worn (29) and that HCWs tended to overuse them out of a sense of protection (24).
The study identified various individual and organizational factors as predictors of knowledge, attitude, and self-reported practice (Table 5). It was found that the older participants had notably better knowledge, in concordance with a study conducted in the United States and Canada (30). It can be explained by their amount of clinical experience and thus the learning opportunities. In our hospital, the staff working in surgery and allied departments were notably more knowledgeable and had better practice. This is in agreement with a study in which respondents from surgery, ICU, and special baby care units had better knowledge scores (12). Considering the perceived risk of infection spread and cross-colonization, it may be due to the regular availability of resources and departmental guidelines. It signified a better attitude and practice of ICU staff, in line with a study conducted among healthcare students (31). A possible explanation can be the need and sensitivity of critical care, due to the use of invasive devices, which is an identified risk factor for acquiring HCAI. A study conducted at military hospitals of Saudi Arabia significantly associated better practice with staff in ICU, gynecology, and obstetrics (32). However, according to WHO guidelines, working in an ICU or surgical care unit and activities with a high risk of cross-contamination have been identified as an observed risk factor for poor adherence (1). A noteworthy finding is a correlation between positive attitude and resident doctors, since residency is a critical period for doctors in shaping lifelong behaviors, attitudes for their professional careers, and optimal patient care. The study also linked positive attitudes to the female gender, supported by a study that revealed female nursing students have significantly better attitudes than male students (17).
The study delineates the knowledge-practice gap in nursing education, which has been widely addressed in literature as principles of practice established in curricula are not well aligned with workplace principles. Regardless, in alignment with a better attitude, 70.65% of the nursing staff had attended formal training on HH in the last 3 years, in comparison with 44.76% of doctors. It is comparable with a study in India, demonstrating significantly more (P < 0.001) nursing students who had received formal training than medical students (8). This can be a plausible explanation for an unusual finding of our study which demonstrated a negative correlation between knowledge and attitude of participants (Table 6).
Self-reported data, descriptive design, and convenience sampling are limitations in this study. Also, the study signifies data from one hospital, thus reducing the generalizability of results. The study did not evaluate the availability of resources and appropriate infrastructure for recommended HH practice. Furthermore, the scope of the study was limited, and compliance with ‘WHO My 5 moments of hand hygiene’ (2) was not evaluated. The sample population despite being adequate was not even across sample characteristics, and thus, some subgroup comparisons could not be derived.
While medical and nursing staff have a moderate knowledge of HH, they differed in attitude and self-reported practice. Healthcare personnel dissatisfaction with training provided, denial of correct practices at all times, lack of feeling guilty after omitting, and disregard of the utility of infection control measures imply the need for multifaceted interventions targeting social, cognitive, and psychological determinants of attitude and behavior for safer patient care.
Conflict of interest and funding
The authors report no conflict of interest. No funding was received for this study.
Ethical approval
The research project was reviewed and assessed by the ethical review committee, CMH Lahore Medical College and Institute of Dentistry, Lahore, Pakistan. The committee had no objection to carrying out this research, and the ethical approval was certified.
References
- Pittet D, Allegranzi B, Sax H, Dharan S, Pessoa-Silva CL, Donaldson L, et al. Evidence-based model for hand transmission during patient care and the role of improved practices. Lancet Infect Dis 2006; 6: 641–52. doi: 10.1016/S1473-3099(06)70600-4
- World Health Organization. WHO guidelines on hand hygiene in health care: a summary first global patient safety challenge clean care is safer care. World Health Organ 2009; 30(1): 270. Available from: http://whqlibdoc.who.int/publications/2009/9789241597906_eng.pdf [cited July 2009].
- World Health Organization. The burden of health care-associated infection worldwide. 2010. Available from: https://www.who.int/gpsc/country_work/burden_hcai/en/ [cited 10 February 2021].
- Prüss A, Giroult E, Rushbrook P. Hospital hygiene and infection control. Safe management of wastes from healthcare activities. Hong Kong: World Health Organization; 1999, pp. 148–58.
- Anwar MA, Rabbi S, Masroor M, Majeed F, Andrades M, Baqi S. Self-reported practices of hand hygiene among the trainees of a teaching hospital in a resource limited country. J Pak Med Assoc 2009; 59: 631–4.
- Kotwal A, Anargh V, Singh H, Kulkarni A, Mahen A. Hand hygiene practices among health care workers (HCWs) in a tertiary care facility in Pune. Med J Armed Forces India 2013; 69: 54–56. doi: 10.1016/j.mjafi.2012.08.011
- Siddarth Sai MS, Srinivas Rao MS, Sandeepthi M, Pavani K, Vinayaraj EV. Hand Hygiene practices among health providers working in tertiary care hospitals in and around Hyderabad, Telangana state (South India). Int J Res Med Sci 2015; 1: 250–5. doi: 10.5455/2320-6012.ijrms20150145
- Whitby M, McLaws M-L, Ross MW. Why healthcare workers don’t wash their hands: a behavioral explanation. Infect Control Hosp Epidemiol 2006; 27: 484–492. doi: 10.1086/503335
- Maheshwari V, Kaore NCM, Ramnani VK, Gupta SK, Borle A, Rituja K. A study to assess knowledge and attitude regarding hand hygiene amongst residents and nursing staff in a tertiary health care setting of Bhopal city. J Clin Diagn Res 2014; 8(8): 4–7. doi: 10.7860/JCDR/2014/8510.4696
- Ather H, Khan A, Shabnum S. Knowledge and compliance toward standard precaution among health care workers at Bahria International Hospital Lahore, Pakistan. Int J Soc Sci Manag 2020; 7(1): 17–20. doi: 10.3126/ijssm.v7i1.27406
- Ahmed J, Malik F, Memon ZA, Bin Arif T, Ali A, Nasim S, et al. Compliance and knowledge of healthcare workers regarding hand hygiene and use of disinfectants: a study based in Karachi. Cureus 2020; 12: 7036. doi: 10.7759/cureus.7036
- Iqbal M, Zaman M, Azam N. Knowledge and perception of hand hygiene among health care workers of a tertiary care military hospital: a descriptive study. Pak Armed Forces Med J 2018; 68(5): 1372–7. Available from: https://www.pafmj.org/index.php/PAFMJ/article/view/2325 [cited 10 February 2021].
- Diwan V, Gustafsson C, Klintz SR, Joshi SC, Joshi R, Sharma M, et al. Understanding healthcare workers self-reported practices, knowledge and attitude about hand hygiene in a medical setting in rural India. PLoS One 2016; 11(10): e0163347. doi: 10.1371/journal.pone.0163347
- Suchitra J, Lakshmi Devi N. Impact of education on knowledge, attitudes and practices among various categories of health care workers on nosocomial infections. Indian J Med Microbiol 2007 Jul 1; 25(3): 181–7. doi: 10.1016/S0255-0857(21)02104-6
- Riasat R, Malik M, Yousaf I, Imam K. Knowledge and practices of infection control among healthcare workers in a tertiary care hospital. Pak J Physiol 2019; 15(4): 46–8. Available from: http://www.pjp.pps.org.pk/index.php/PJP/article/view/1190 [cited 10 February 2021].
- World Health Organization. Hand hygiene knowledge questionnaire for health-care workers. 2009. World Health Organization, Geneva.
- Cruz J, Cruz C, Al-Otaibi ASD. Gender differences in hand hygiene among Saudi nursing students. IJIC 2015; 11(4). doi: 10.3396/ijic.v11i4.029.15
- Goyal A, Narula H, Gupta P, Sharma A, Bhadoria A, Gupta P. Evaluation of existing knowledge, attitude, perception and compliance of hand hygiene among health care workers in a Tertiary care centre in Uttarakhand. J Fam Med Prim Care 2020; 9(3): 1620. doi: 10.4103/jfmpc.jfmpc_1183_19
- Squires JE, Linklater S, Grimshaw JM, Graham ID, Sullivan K, Bruce N, et al. Understanding practice: factors that influence physician hand hygiene compliance. Infect Control Hosp Epidemiol 2014 Dec; 35(12): 1511–20. doi: 10.1086/678597
- Barroso V, Caceres W, Loftus P, Evans KH, Shieh L. Hand hygiene of medical students and resident physicians: predictors of attitudes and behaviour. Postgrad Med J 2016; 92(1091): 497–500. doi: 10.1136/postgradmedj-2015-133509
- Vaillant L, Birgand G, Esposito-Farese M, Astagneau P, Pulcini C, Robert J, et al. Awareness among French healthcare workers of the transmission of multidrug resistant organisms: a large cross-sectional survey. Antimicrob Resist Infect Control 2019; 8(1): e173. doi: 10.1186/s13756-019-0625-0
- Alfahan A, Alhabib S, Abdulmajeed I, Rahman S, Bamuhair S. In the era of corona virus: health care professionals’ knowledge, attitudes, and practice of hand hygiene in Saudi primary care centers: a cross-sectional study. J Community Hosp Intern Med Perspect 2016 Jan; 6(4): 32151. doi: 10.3402/jchimp.v6.32151
- Yehouenou CL, Dohou AM, Fiogbe AD, Esse M, Degbey C, Simon A, et al. Hand hygiene in surgery in benin: opportunities and challenges. Antimicrob Resist Infect Control 2020; 9(1): 85. doi: 10.1186/s13756-020-00748-z
- Jang T-H, Wu S, Kirzner D, Moore C, Youssef G, Tong A, et al. Focus group study of hand hygiene practice among healthcare workers in a teaching hospital in Toronto, Canada. Infect Control Hosp Epidemiol 2010; 31(2): 144–50. doi: 10.1086/649792
- Sili U, Ay P, Bilgin H, Hidiroglu S, Korten V. Hand hygiene knowledge, perception and practice of healthcare workers in a Turkish university hospital intensive care unit. J Infect Dev Ctries 2019 Aug 31; 13(8): 744–7. doi: 10.3855/jidc.10916
- Phan HT, Tran HTT, Tran HTM, Dinh APP, Ngo HT, Theorell-Haglow J, et al. An educational intervention to improve hand hygiene compliance in Vietnam. BMC Infect Dis 2018; 18(1): e116. doi: 10.1186/s12879-018-3029-5
- Sopjani I, Jahn P, Behrens J. Training as an effective tool to increase the knowledge about hand hygiene actions. An evaluation study of training effectiveness in Kosovo. Med Arch 2017; 71(1): 16–19. doi: 10.5455/medarh.2017.71.16-19
- Akingbola OA, Singh D, Srivastav S, Plunkett DS, Combs MM. The Impact of Hand Hygiene Posters on Hand Hygiene Compliance Rate among Resident Physicians: A Brief Report. Clinical Pediatrics 2016; 1(4): 1–2. doi: 10.4172/2572-0775.1000113.
- Fuller C, Savage J, Besser S, Hayward A, Cookson B, Cooper B, et al. ‘The dirty hand in the latex glove’: a study of hand hygiene compliance when gloves are worn. Infect Control Hosp Epidemiol 2011; 32(12): 1194–9. doi: 10.1086/662619
- Kirk J, Kendall A, Marx JF, Pincock T, Young E, Hughes JM, et al. Point of care hand hygiene – where’s the rub? A survey of US and Canadian health care workers’ knowledge, attitudes, and practices. Am J Infect Control 2016; 44: 1095–110. doi: 10.1016/j.ajic.2016.03.005
- Elsafi S, Al-Howti S. Factors influencing hand hygiene compliance of healthcare students. IJIC 2019; 15(4): e19118. doi: 10.3396/ijic.v15i4.015.19
- ALSofiani AM, AlOmari F, AlQarny M. Knowledge and practice of hand hygiene among healthcare workers at Armed Forces Military Hospitals, Taif, Saudi Arabia. Int J Med Sci Public Health 2016; 5(6): 1282. doi: 10.5455/ijmsph.2016.15042016439