ORIGINAL ARTICLE
Preparation of operating room for COVID-19 suspects at a tertiary care teaching hospital in New Delhi, India
Jitender Sodhi1, Anant Gupta1*, Gurpreet Singh1, Gagandeep Singh2, Rajeev Kumar3, Arti Kapil2 and Peush Sahni4
1Department of Hospital Administration, All India Institute of Medical Sciences, New Delhi, India; 2Department of Microbiology, All India Institute of Medical Sciences, New Delhi, India; 3Department of Urology, All India Institute of Medical Sciences, New Delhi, India; 4Department of Gastrointestinal Surgery and Liver Transplantation, All India Institute of Medical Sciences, New Delhi, India
Abstract
The continuous rise in the number of cases of COVID-19, caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), generated an urgent need to transform the facilities of our existing operating rooms (OR) to cater for emergency surgeries for patients with suspected COVID-19. The aim was to minimise the spread of infection and to achieve the lowest risk for patients and staff while caring for COVID-19 suspects undergoing surgery. We devised a protocol in our hospital to prepare OR for patients suspected to be suffering from COVID-19 but in whom the surgical intervention could not be deferred until the result of the COVID-19 test was obtained. The key consideration was that we cater to suspected and confirmed COVID-19 patients who required emergency surgery while adhering to strict infection control measures. The study was undertaken as a pilot exercise in consultation with treating surgeons, hospital infection control committee members, hospital administrators, and engineers, along with a literature review, to transform the design and functioning of existing facilities to prepare for emergency surgeries of COVID-19 suspects at the beginning of the pandemic. While this required significant planning on paper and onsite by members of the OR staff, hospital infection control committee, administration, and engineers, the creation of a safe operating environment was possible within a 48-h period with minimal structural alterations.
Keywords: Operating rooms; COVID-19; infection control; human resources; India
Citation: Int J Infect Control 2022, 18: 21395 – http://dx.doi.org/10.3396/ijic.v18.21395
Copyright: © 2022 Jitender Sodhi et al. This is an Open Access article distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for any purpose, even commercially, provided the original work is properly cited and states its license.
Received: 1 March 2021; Revised: 11 August 2021; Accepted: 21 September 2021; Published: 30 May 2022
Competing interests and funding: The authors have no conflicts of interest. The authors have not received any funding or benefits from industry or elsewhere to conduct this study.
*Anant Gupta, Department of Hospital Administration, All India Institute of Medical Sciences, New Delhi, India. Email: anant933@gmail.com
The World Health Organization (WHO) declared COVID-19, the disease caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), a global pandemic on 30 January 2020 (1). On the same date, India reported its first case of COVID-19, and from then onwards, case numbers were on a continuous rise. From 25 March 2020, the whole country was placed under a complete lockdown with healthcare services rendered on a reduced scale. The COVID-19 pandemic underlines the importance of meticulous planning of our existing facilities to ensure judicious use of financial and human resources. It is important that we cater to suspected and confirmed COVID-19 patients who require emergency surgery while adhering to strict infection control measures. To minimise the spread of infection and to achieve the lowest risk for patients and staff while caring for COVID-19 suspects undergoing surgery, we devised a protocol in our hospital to prepare operating rooms (ORs) for patients suspected to be suffering from COVID-19 but in whom the surgical intervention could not be deferred until the result of the COVID-19 test was obtained.
Location of OR
Our ORs are located on the 8th and top floor of the main hospital building of a tertiary care teaching hospital in an urban area of New Delhi, India, with a bed capacity of 2,486 beds. The ORs of the main hospital building cater for approximately 17,000 surgeries per year. All ORs are in one row with a clean external corridor, a row of changing rooms, and an internal corridor followed by the row of ORs (Fig. 1). There are gates for entry into the central corridor at each end and in the centre. Elevators are available at both ends and at the centre of the corridor to connect to the rest of the hospital. A single air handling unit (AHU) caters to three consecutive ORs within the block.
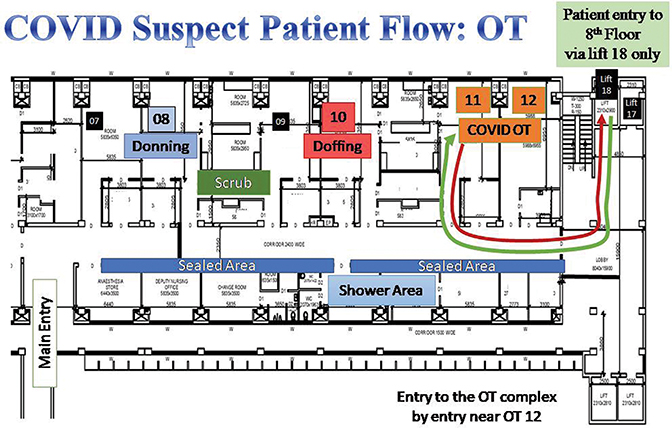
Fig. 1. Flow of COVID suspect patients in the OR complex. Green arrow represents movement of the patient into the OR area. Red arrow represents movement of the patient out of the OR. (OT=operating room)
Selection of OR
It was decided to convert one of the blocks of the existing ORs between the central and terminal exits into the COVID suspect wing. This block includes six ORs with two sets of three ORs having their own AHUs. The criteria for the selection of ORs were based on the following: (1) possibility of segregating access through an elevator earmarked for these patients; (2) minimal transport and movement inside the OR; (3) ease of handing/taking over of patient; and (4) possibility of isolating the heating, ventilation, and air conditioning unit (HVAC). Within this block, the three terminal-end ORs have an HVAC, and it was possible to create a negative pressure environment. It was decided that these would serve as the functional ORs, while the three centrally located ORs would be designated for donning, doffing, and entry of healthcare workers (HCWs). The elevators at the terminal end would serve to bring in the patient, and patient entry would be through that end, diametrically opposite the entry of HCWs.
Patient transport
We defined a dedicated route for the vertical transport of COVID-19 suspected patients to the OR, keeping it as short as possible and away from other patients and people in general within the hospital to minimise the risk of infection. One elevator at the terminal end, adjacent to entry into the OR, was designated as the COVID-19 lift. It was reprogrammed to halt only at designated places and served to transport patients admitted from emergency into the designated wards on the 3rd and 6th floors, and to the OR and back to the admission wards (Fig. 1).
Preparation of equipment
Equipment stored in the inner corridor was cleared to enable cleaning and infection control. Equipment kept inside the ORs was minimised to the expected requirements for emergency surgeries. Extra equipment was kept in the clean areas but could be brought in if required. Standard anaesthesia trolleys were replaced with dedicated pre-prepared ones with minimal but adequate stock. All surgical instruments for the planned surgery were pre-emptively prepared and brought into the OR prior to wheeling in the patient. We emphasised the use of disposable material wherever possible. Equipment for delivery including a baby warmer was kept in the designated area.
Team movement
The minimum number of operating team members essential for a given surgery would be donned. During surgery, the minimum movement of staff in and out of the OR was ensured to reduce the risk of infection. The flow of movement of the operating team was piloted and finalised through a dry run, in consultation with members of the Hospital Infection Control Committee (HICC). At any point in time, only one suspect OR would be functional, meaning that the scrubbed operating team was either inside the OR or leaving the OR for doffing, thus minimising the possibility of an encounter of a scrubbed team member with one going for doffing. The key considerations in the planning were (a) entry of OR team through one end and entry of patient (wheeling in) from the opposite end, (b) minimum travel distance between the doffing room and the changing room, and (c) no back movement of anyone behind the doffing area (Fig. 2).
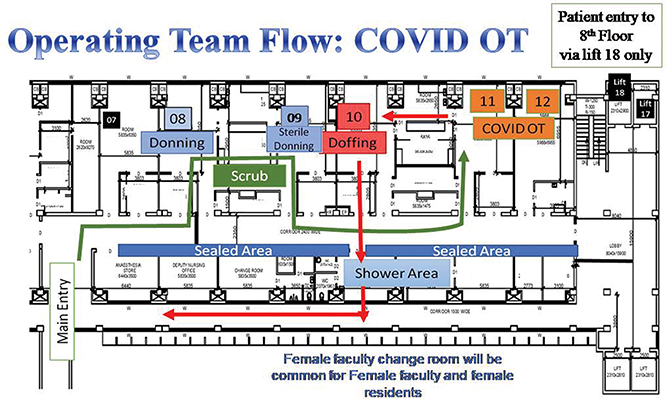
Fig. 2. Flow of OT staff in the OR complex. Green arrow represents movement of the staff into the OR area. Red arrow represents movement of the staff out of the OR. (OT=operating room)
Donning and doffing
The designated donning and doffing areas are marked in Fig. 2. Level 3-type personal protective equipment kits that included an impervious coverall, Respirator N95 mask or filtering facepiece respirator (FFP) 2, face shield, goggles, sterile gloves, gumboots (where required), and long shoe covers (impervious type) were made available in the donning area. To ensure that the correct process of donning and doffing was followed, checklists were provided by the HICC in both areas. In the doffing area, a buddy system was ensured to observe and facilitate the correct process of doffing of the operating team member. We ensured that two pairs of clean and dirty chairs were kept in a row where one member would sit on the dirty chair, doff, go to the clean chair, and finally exit (Table 1).
Table 1. Workflow and preparation of operating rooms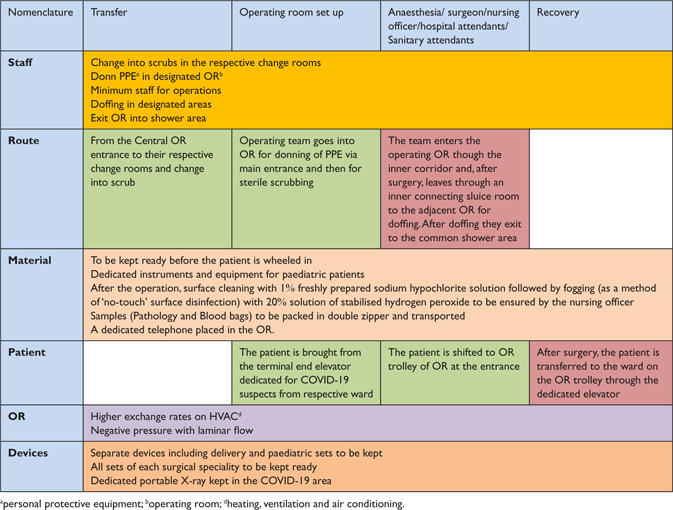
HVAC considerations
Conventionally good ventilation, low humidity (<68%), and temperature control should be maintained in the OR for the comfort of surgical personnel and patients and also for preventing infections (2). OR should be maintained at positive pressure with respect to corridors and adjacent areas (3). The positive pressure restricts the movement of air from outside areas into the OR and thus decreases the risk of infection being brought into the OR. Conventional OR ventilation systems produce a minimum of 15 air changes of filtered air for thermal control, three (20%) of which must be fresh air. Air should be introduced at the ceiling and exhausted near the floor (4).
While ORs are normally designed to have positive pressure air circulation, while operating on COVID-19 patients, negative pressure is recommended inside the OR to minimise the risk of infection going from inside the OR to the clean air outside (5–7). The ORs in our setting open directly into the central corridor; however we have an anaesthesia induction room in each OR which is kept at negative pressure. With each AHU catering to three ORs, including their changing rooms outside these ORs, there was no provision in our setting to partition and segregate the inside air of ORs at a different pressure through an anteroom. Therefore, it was required to keep the ORs at negative pressure in order to prevent the mixing and transmission of air from inside of these ORs. A high air exchange cycle rate (≥25 cycles/h) contributes to effectively reducing the viral load within ORs (6, 8, 9). To achieve this, the inlet flow was reduced and the exhaust speed was increased, which created a relative negative pressure in the OR in comparison with the corridors. The laminar flow was maintained and was also tested after the changes; the air flowed from the ceiling to the scrub area. The ducts of the HVAC supplying the changing rooms and external corridors were closed, and the doors of these rooms facing the corridors were sealed. These actions minimised the risk of infection being carried from inside the OR to the changing rooms or the clean areas outside.
Other engineering considerations
Certain civil structural modifications were also required. Entry into the block of six ORs was sealed with acrylic sheets with leak-proof structures from both the ends to restrict air flow into non-COVID ORs and the clean corridors. Air vents and doors of changing rooms facing the central corridor opposite the block of three working ORs were sealed as these were served by the same HVAC as the ORs. All the exhaust fans in these changing rooms were electrically disconnected, and all the vents in these rooms were closed physically to ensure that air movement was practically cut off across the inner corridors. The changing rooms were refurbished by the installation of showers and geysers so that operating team members could take a shower after doffing.
Infection control measures
From the infection control point of view, the equipment dedicated for the surgery of COVID-19 suspects was kept separately. The route and trolley were designated for the transport of patients from the ward, and every time the trolley left the OR, it was wiped with hypochlorite solution. The blood sample, if any, was transported in a double bag, wiped with hypochlorite solution. The HVAC was kept at negative pressure. After each operation, the equipment was cleaned in the sluice room, and the OR was cleaned with disinfectant followed by its fogging, which was performed using hydrogen peroxide for a contact period of an hour.
As a limitation of the study, we cannot provide outcomes data as this study was not planned to collect them. The study was undertaken as a pilot exercise in consultation with the treating surgeons, HICC members, hospital administrators, and engineers along with a literature review to transform the existing facility in its design and functional aspects to make it ready for the emergency surgeries of COVID-19 suspects at the beginning of the pandemic.
Summary
While this required significant planning on paper and onsite by members of the OR staff, HICC, administration, and engineers, the creation of a safe operating environment was possible within a 48-h period with minimal structural alterations.
Acknowledgement
We would like to thank our anaesthesia colleagues, the operating room nurses, technicians, and other staff without whom this study would not have been possible.
Ethical approval
Ethical consideration for this study is not applicable.
Authors’ contributions
Jitender Sodhi was involved in the conceptualisation of the plan, preparation of the manuscript, and execution of the work and provided inputs on various design aspects. Anant Gupta was involved in the conceptualisation of the plan, preparation of part of the manuscript, and execution of the work and provided inputs on HVAC aspects. Gurpreet Singh was involved in the execution of the work and provided inputs on engineering aspects. Gagandeep Singh provided inputs on infection control and manuscript review. Rajeev Kumar was involved in the conceptualisation of the plan and manuscript review and provided inputs on various design aspects. Arti Kapil provided inputs on infection control and manuscript review. Peush Sahni was involved in the conceptualisation of the plan and manuscript review, provided inputs on various design aspects, and gave overall mentorship.
References
- World Health Organization. Statement on the second meeting of the International Health Regulations (2005) Emergency Committee regarding the outbreak of novel coronavirus (2019-nCoV). Available from: https://www.who.int/news-room/detail/30-01-2020-statement-on-the-second-meeting-of-the-international-health-regulations-(2005)-emergencycommittee-regardingthe-outbreak-of-novel-coronavirus-(2019-ncov) [cited 7th March 2020].
- Everett WD, Kipp H. Epidemiologic observations of operating room infections resulting from variations in ventilation and temperature. Am J Infect Control 1991; 19: 277–82. doi: 10.1016/0196-6553(91)90173-A
- Lidwell OM. Clean air at operation and subsequent sepsis in the joint. Clin Orthop 1986; 211: 91–102. doi: 10.1097/00003086-198610000-00013
- Nichols RL. The operating room. In: Bennett JV, Brachman PS, eds. Hospital infections, 3rd ed. Boston, MA: Little, Brown and Company; 1992, pp. 461–73.
- Grelat M, Pommier B, Portet S, Amelot A, Barrey C, Leroy H-A, et al. Patients with Coronavirus 2019 (COVID-19) and Surgery: Guidelines and Checklist Proposal. World Neurosurgery 2020; 139: e769–73. doi: 10.1016/j.wneu.2020.04.155
- Chow TT, Kwan A, Lin Z, Bai W. Conversion of operating theatre from positive to negative pressure environment. J Hosp Infect 2006; 64: 371–8. doi: 10.1016/j.jhin.2006.07.020
- Park J, Yoo SY, Ko J-H, Lee SM, Chung YJ, Lee J-H, et al. Infection Prevention Measures for Surgical Procedures during a Middle East Respiratory Syndrome Outbreak in a Tertiary Care Hospital in South Korea. Sci Rep 2020; 10: 325. doi: 10.1038/s41598-019-57216-x
- Ti LK, Ang LS, Foong TW, Ng BSW. What we do when a COVID-19 patient needs an operation: operating room preparation and guidance. Can J Anaesth 2020; 67: 756–8. doi: 10.1007/s12630-020-01617-4
- Wong J, Goh QY, Tan Z, Lie SA, Tay YC, Ng SY, et al. Preparing for a COVID-19 pandemic: a review of operating room outbreak response measures in a large tertiary hospital in Singapore. Can J Anaesth 2020; 67: 732–45. doi: 10.1007/s12630-020-01620-9