ORIGINAL ARTICLE
Knowledge, perception of risk of disease, and infection prevention and control practices among healthcare workers and support staff toward COVID-19 in an Ethiopian referral hospital: a cross-sectional survey
Esubalew T. Mindaye*, Bekalu Assaminew and Goytom K. Tesfay*
Department of Surgery, St. Paul’s Hospital Millennium Medical College, Addis Ababa, Ethiopia
Abstract
Coronavirus disease 2019 (COVID-19) is a pandemic affecting over 106 million and killing over 2.3 million people. Inadequate knowledge of the disease coupled with scarce or improper use of infection prevention and control (IPC) measures by healthcare workers (HCWs) and support staff may be contributing to the rapid spread of infection. This survey aims to assess knowledge, risk perception, and precaution practices of HCWs and support staff toward COVID-19 under resource-constrained circumstances at a major referral hospital in Ethiopia. An institution-based survey was conducted in April 2020 using 422 subjects selected by stratified random sampling. A five-section survey instrument was distributed, and the collected responses were cleaned and entered into Epi data (v3.1) and exported to SPSS (v.26) for further statistical analysis. The survey found that about 58% of the HCWs and support staff in the hospital appear to have adequate awareness and perceive COVID-19 to be a high-risk disease. Seven out of 10 subjects practice some form of IPC measures. However, the knowledge among allied HCWs and support staff appears to be inadequate. Gender, occupation, and years in service correlated with the level of awareness. Of those surveyed, 78% were concerned about the lack of personal protective equipment and perceived public transportation to be a high-risk factor for the transmission of infection. Additional campaigns may be necessary to reinforce existing knowledge of HCWs, but more emphasis should be geared toward educating allied HCWs and support staff.
Keywords: COVID-19; pandemic; survey; knowledge; occupational exposure; Ethiopia
Citation: Int J Infect Control 2021, 17: 20726 – http://dx.doi.org/10.3396/ijic.v17.20726
Copyright: © 2021 Esubalew T. Mindaye et al. This is an Open Access article distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for any purpose, even commercially, provided the original work is properly cited and states its license.
Received: 20 August 2020; Revised: 9 February 2021; Accepted: 15 February 2021; Published: 4 June 2021
Competing interests and funding: We confirm that we declare no conflict of interest. We also did not receive funding or benefits from industry to conduct this study.
*Esubalew T. Mindaye, Department of Surgery, Saint Paul’s Hospital Millennium Medical College, Swaziland Street, P.O. Box 1271, Addis Ababa, Ethiopia. Email: esubetad24@yahoo.com
*Goytom Knfe Tesfay, Department of Surgery, Saint Paul’s Hospital Millennium Medical College, Swaziland Street, P.O. Box 1271, Addis Ababa, Ethiopia. Email: knfegoytom@gmail.com
To access the supplementary file, please visit the article landing page
Coronaviruses are respiratory viruses that are known to cause illness ranging from the common cold to severe acute respiratory syndrome (1). The transmission is mainly by respiratory droplets and direct and indirect contacts. Airborne transmission other than that by aerosol generating procedures and feco-oral transmission routes are yet to be confirmed. Most coronaviruses infect animals and the transmission from bats to humans might have occurred after mutation via an intermediate host(s), but as yet there is no definitive host identified for coronavirus disease 2019 (COVID-19). Severe acute respiratory syndrome (SARS) in 2002 killed 800 people (case fatality rate [CFR] of 10%), and in 2012, Middle East respiratory syndrome (MERS) killed 860 people (CFR of 40%) (2). Recently, a novel coronavirus was isolated from the lower respiratory tract of patients who were suffering from pneumonia in Wuhan, Hubei Province, China. The World Health Organization (WHO) declared COVID-19 as a public health emergency of international concern on January 30, 2020, and then later on March 11, 2020, as a pandemic (3, 4). As of February 08, 2021, there are more than 106 million confirmed cases with more than 2.3 million deaths globally. Out of the confirmed cases, more than 3.6 million cases are in the African continent. The first reported case in Ethiopia was on March 12, 2020, and since then, the confirmed cases reached 136,365 (January 29, 2021) with 2,087 fatalities. This number may be an underestimation of the cases in Ethiopia because testing is limited (5).
In the absence of effective antiviral treatment or vaccine, prevention is the key to control the spread (2). Healthcare workers (HCWs) are at increased risk of acquiring COVID-19 at workplace, especially in resource-limited countries (6). On September 2, the WHO Pan American Regional Office in Washington, DC, reported that 570,000 HCWs were infected and 2,500 patients were dead due to COVID-19 (7). In one case study, nearly 29% of the affected patients were HCWs, and hospitals were the presumed place of exposure. Some died of complications and many more were quarantined after exposure to a suspected or confirmed case of COVID-19 (8). The high contagion, asymptomatic persons or atypical presentation, inadequate and delayed testing of suspected cases, improper use or inadequate supply of personal protective equipment (PPE), and other preventive measures against coronavirus increase the likelihood of HCWs being infected (6, 9, 10). In developing countries, infection of HCWs would significantly undermine the fragile healthcare system by stretching an already thin workforce. Besides, the possibility of catching the virus and spreading it to vulnerable family members such as the elderly could affect the overall willingness of HCWs to work during an outbreak. Recognizing this as a concern, the WHO and the US Centers for Disease Prevention and Control (CDC) have prepared manuals with recommendations and started providing free online training. The confirmed cases in Ethiopia are increasing and so is the risk to frontline HCWs and their families.
Most studies conducted on COVID-19 focus on the clinical characteristics and epidemiology of the disease and not on its relation to HCWs. There is an urgent need to evaluate and improve the level of awareness of HCWs. Thus, we aim to explore knowledge, perception of risk, and the infection prevention and control (IPC) practices of HCWs and support staff against COVID-19 in a tertiary teaching hospital in Ethiopia. The findings of this survey are expected to identify strengths and weaknesses of the current IPC practices in the survey hospital, increase awareness of policy makers and national programs about preventive measures, serve as a baseline study, and supplement other studies on the subject of COVID-19 to galvanize the effort to control the spread of the disease.
Materials and methods
Study design
The survey was conducted at St. Paul’s Hospital Millennium Medical College (SPHMMC) in Addis Ababa, which is the second-largest multi-specialty tertiary care teaching hospital in Ethiopia. The hospital has been giving medical services for more than 50 years with an emphasis on the underserved population. There are about 800 students and more than 3,031 medical staff (11). The cross-sectional survey was conducted from March 30 to May 2020. Participants were drawn from all healthcare professionals and support staff actively working in the hospital for at least 6 months. Workers on personal, sick, or maternity leave were excluded.
Sample size determination and sampling technique
Sample size was calculated based on a prior presumption that the proportion (P) of HCWs and support staff with adequate knowledge on COVID-19 would be about 50% with the desired precision of d = 0.05. The sample size was determined using the single population proportion formula and adding nonresponse rate of 10%. Using stratified random sampling, 422 subjects were included in the survey. The variables assessed were risk perception, self-reported IPC practices, and knowledge about COVID-19.
Data collection and scoring
Data were collected using a self-administered semi-structured questionnaire that was prepared after a thorough literature review on COVID-19. The scope and structure of the questionnaire are included in the Supplement. We tried to objectively assess the knowledge of HCWs about the disease using structured questions focusing on COVID-19 etiology, symptoms, transmission, and treatment. Each response was recorded as ‘yes’ or ‘no’ and transformed into scores ranging from 0 to 28. Knowledge scores for individuals were calculated and summed up to give the total knowledge score. The risk perception and self-reported practice statements were scored on a 5-point Likert scale, from 1 to 5 (strongly agree 5, agree 4, neutral 3, disagree 2, and strongly disagree 1). To calculate the overall risk perception, responses were scored on a 0–12 range with a score > 9 (80%) considered as high-risk perception. The results of each practice related question were summed up to give a score of 0–35. Testing of the questionnaire was carried out in 21 (5%) randomly selected HCWs and support staff from their respective departments. Following input, the questionnaire was distributed to the study population. Both paper-based and online Google forms-based questionnaires were used to collect data. Participants were given sufficient time to read, comprehend, and answer all the questions; and information about the survey was provided to address any question.
Data processing and analysis
The processing began by checking the gathered data for accuracy and completeness. Each completed questionnaire was assigned a unique code and entered into Epi Info version 3.5.1 (CDC, Atlanta, GA, USA) and exported to SPSS version 26 (IBM, Armonk, NY, USA) for further analysis. Results are presented as frequency distributions, cross-tabulations, and graphs. Continuous variables are presented as mean and standard deviation (SD), and categorical variables are presented as frequency and percentages. The chi-square test was used to evaluate the level of association. Statistical significance was established at a P-value of <0.05. Operational definitions and cut-off points used in this survey are provided in the Supplement.
Ethical clearance
Clearance was obtained from the Institutional Research and Ethics Review Committee (IRB) of the SPHMMC. Participation of the HCWs in the study was voluntary.
Results
Socio-demography
With a response rate at 100%, 422 study subjects participated in the survey of whom 339 were HCWs and 83 were support staff (Table 1 and Supplementary Material). The gender composition was 47% male and 53% female with an overall average age of 27.6 years. More than half of them have served in the hospital for at least 2 years. About 74% were using public transport (taxi and bus) to travel to and from work, and most were living with their nuclear family.
Knowledge and source of information of the participants
All participants stated to have heard about COVID-19, and 66% (278) of them had the opportunity to attend formal training sessions/lectures about COVID-19 at some point. About 69% of the participants thought that they had sufficient information about COVID-19 and its prevention (Fig. 1a and b). As shown in Fig. 1c, doctors self-reported using official websites (WHO, CDC, or Ethiopian Federal Ministry of Health [FMOH]) as their main source of information followed by social and mass media. Allied HCWs used official websites and mass media equally as the main source. However, the support staff was getting COVID-19-related information primarily from mass media and social media.
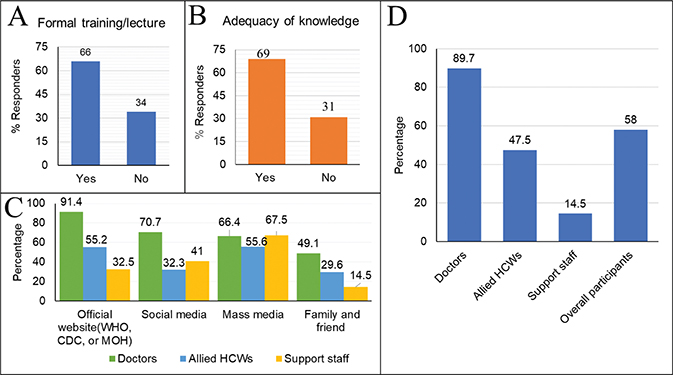
Fig. 1. Knowledge and sources of COVID-19 information among participants. (a) Formal training about COVID-19. (b) Adequacy of knowledge (self-assessment) among HCWs and support staff. (c) Sources of information about COVID-19. (d) Percentage of HCWs and support staff with adequate knowledge (score > 80%).
As summarized in Fig. 1d, doctors received the highest score with nearly 90% of them having adequate knowledge about COVID-19 (score > 22 out of 28 or 80%). Based on their responses, about 48% of the allied HCWs appeared to have adequate knowledge, and support staff scored the lowest with 14.5%. Overall, about 58% of the participants had knowledge surpassing the 80% adequacy threshold. The mean knowledge score for HCWs and support staff was about 82 and 60%, respectively.
Further granular detail of knowledge of HCWs was assessed and summarized in Table 2. Nine out of 10 doctors and 61% of the allied HCWs said that SARS-CoV-2 is the cause of COVID-19 but only 36% of the support staff answered this question correctly. About 82% of doctors identified the origin of SARS-CoV-2 to be bats, while 48.4 and 59% of the allied HCWs and support staff, respectively, said the same about the origin. Doctors, allied HCWs, and support staff identified fever (99.1, 86.5, 66.3%) and cough (98.3, 70.9, 69.9%) as the most common symptoms that COVID-19 patients might manifest. The majority of the participants identified droplets and contact to be known modes of transmission, and over 50% of doctors believed that feco-oral transmission is possible. Nine out of 10 doctors and 80% of the allied HCWs understood that asymptomatic transmission is a possibility, while only 23% of the support staff knew about asymptomatic transmission.
Perception of risk
The overwhelming majority of HCWs was fearful of acquiring COVID-19 at the workplace (Table 3). Over 97% of physicians, 91% of allied HCWs, and 88% of support staff said they likely or very likely expected to be infected in hospital at some point, and more than 80% of the workers were concerned that they may transmit the virus to family members. The perception about the fatality from COVID-19 varied among respondents with the majority of hospital support staff perceiving COVID-19 to be highly fatal (86%). At least 80% of physicians responded that there is a good chance of surviving this disease if infected. Overall, the perceived risk and the ability to recover from COVID-19 appeared to be associated with the degree of involvement in patient care and the level of training of the professional. Over 58% (244) of the HCWs and support staff perceived COVID-19 to be a high-risk disease.
The practice of preventive measures against COVID-19
The majority of HCWs and support staff reported practicing IPC measures. As depicted in Fig. 2a, nearly 90% of HCWs and 80% of support staff agreed or strongly agreed that they avoided shaking hands and large-group gatherings. Similarly, 86% of the respondents covered their noses when coughing or sneezing, and 89% of the respondents washed their hands after exposure to respiratory secretions. Over 54% of the respondents used public transport to and from the hospital and considered this a high-risk factor. Of the respondents, 78% (313) agreed or strongly agreed that there was inadequate PPE available at their current workplace, while 16% (66) felt that the PPE availed to them was adequate. In regard to practicing the WHO’s 5 Moments for Hand Hygiene, 76% of the HCWs reported that they performed handwashing at all five moments, while 82 and 87% of the HCWs practiced washing before and after touching a patient, respectively (Fig. 2b). The overall practice of preventive measures against COVID-19 was assessed by asking seven Likert scale questions (Fig. 2c). With the arbitrary score of ≥ 26 (75%) considered as good, 74% (311) of the participants scored 75% or more in the self-reported practice of precautionary measures.
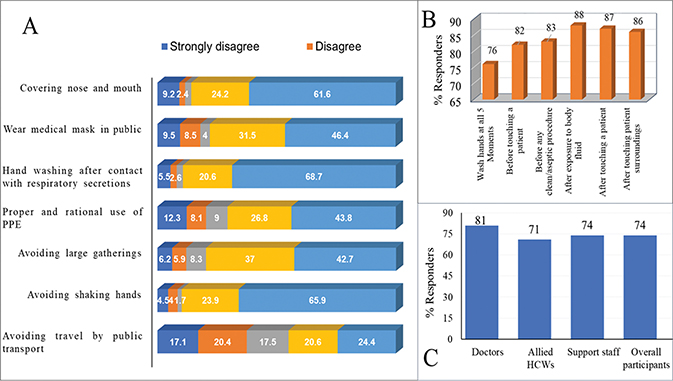
Fig. 2. Self-reported infection prevention and control practices for COVID-19. (a) Stacked bar in percentage of HCWs’ and support staffs’ responses to the practice questions (n = 422). (b) Percentage of HCWs’ reported handwashing practices for the WHO’s five moments of handwashing (n = 339). (c) The practice of preventive measures by the HCWs and support staff.
The role of respondents’ attributes to knowledge, risk perception, and the practice of preventive measures
Table 4 shows that people with more years in healthcare service tended to practice IPC measures more frequently (P-value 0.019). A statistically significant association was observed between occupation or gender and knowledge about COVID-19. It is counterintuitive that factors such as training about COVID-19 neither improved the understanding about the disease (P = 0.645) nor improved the practice of IPC measures (P = 0.608). Similarly, living circumstances at home appear to have an insignificant effect on knowledge, perception of risk, and practice of preventive activities.
| Respondents by attribute | Knowledge | Risk perception | Practice | |||
| P | Cramer’s V/Phi* | P | Cramer’s V/Phi | P | Cramer’s V/Phi | |
| Occupation | 0.000** | 0.586 | 0.266 | 0.137 | ||
| Year of service | 0.016** | 0.170 | 1 | 0.019** | 0.128 | |
| Marital status | 0.404 | 0.577 | 0.897 | |||
| Gender | 0.000** | 0.225 | 0.216 | 0.261 | ||
| Living circumstances | 0.537 | 0.150 | 0.608 | |||
| Training | 0.645 | 0.654 | 0.107 | |||
| *Cramer’s V/Phi values shown are only for those shown to have significant association on the chi-square test. **The factors with significant association. |
||||||
Free-text responses
One hundred and eight respondents (25%) made at least one free-text comment. The responses were predominantly about the shortage of PPE for use during hospital hours. Many respondents commented that they had to use public transport to and from the hospital in crowded buses and taxis, endangering themselves, their families, and the public. It is noteworthy that many responded that they take pride in and obtain great joy from their job and are willing to help patients. However, they also expressed frustration and pressure because of perceived ‘lack of value’ afforded to their well-being.
Discussion
COVID-19 is an emerging and rapidly changing pandemic with a wide-ranging impact on global healthcare systems and other aspects of human life. Both the HCWs and hospital support staff are at the forefront of the fight against COVID-19 and are affected by the disease. In the context of resource-constrained countries, the likelihood of them acquiring the disease is higher compared to the general population (6, 12, 13). This is partly due to the fact that PPE is scarcely available, and at times, the quality or effectiveness of PPE for HCWs is not necessarily at par with the transmissibility of this virus. Adequate knowledge about clinical manifestations, diagnosis, management, and established IPC measures is important in the fight to contain its spread. In this survey, we set out to evaluate the knowledge, perception of risk of the disease, and self-reported IPC practices of HCWs and support staff toward COVID-19. We found that the mean knowledge score of HCWs and support staff was about 82 and 60%, respectively. These scores are comparable to studies done elsewhere in an African hospital (82.4%) and US residents (80%) (12, 14). However, the mean score is slightly lower than among Chinese residents (90%) (15). This might be partly because the survey was done at an earlier phase of the pandemic in Ethiopia or can be attributable to the limited access to information sources and IPC facilities in Ethiopia. COVID-19 is yet to be fully understood, and thus, objective evaluation of the adequacy of knowledge about the disease is a challenge. Despite the limitation, we found that about 58% of the respondents appeared to have adequate knowledge about COVID-19. This observation is in line with previous findings of a study by Olum et al. (12) among the HCWs of Makerere Hospital, Uganda, which is 69%, and with the results of a survey 58.7%, by Bhagavathula et al. in the United Arab Emirates (10). However, this score is much lower than what was reported by Huynh et al. in Vietnam, which was around 88.4% (16).
It appears there is difference in knowledge between HCWs and support staff with 90% of medical doctors commanding adequate knowledge about COVID-19, while a sizable portion of allied health workers including nurses lacked knowledge in a certain area of the disease. Moreover, only 14% of the support staff were equipped with the necessary knowledge about the disease (score ≤ 80%) with the majority falling short in some key elements of prevention of COVID-19 and the lowest scores being for hospital cleaners. This might be alarming because these workers are highly vulnerable to healthcare-associated infection with consequent transmission to other HCWs and their families.
The mean perception of risk by all HCWs was around 58%, which appears to be higher than some other findings. For example, in Germany, the risk perception among the general population was about 34% (17). The difference in risk perception might be attributable to the target study subjects (hospital workers in the current survey as opposed to the general German population). Furthermore, the majority of respondents were anxious that COVID-19 is a high-risk disease for themselves (92%) or their families (86%). The anxiety of HCWs is in agreement with the results of the study in China that reported around 85% (18). In another study, 92% of HCWs in Iran were afraid of being infected with the disease and transmitting it to their family (19). Owing to the perceived risk, the majority of surveyed HCWs in this survey (74%) reported practicing IPC measures. These measures include regular hand hygiene, social distancing, avoiding crowded places and large gatherings, wearing a facemask, covering mouth and nose while coughing or sneezing, and avoiding handshaking. Comparable studies showed IPC practices follow the same trend as in Uganda or Saudi Arabia (12, 20). In contrast, nearly 90% of HCWs in China regularly practice preventive measures (18). The will to practice preventive measures will likely be undermined by a shortage of PPE in the hospital. The majority of surveyed HCWs (78%) reported their concern for lack of PPE (facemasks, shields, and gloves). At the time of this survey, about 77% HCWs and 83% support staff regularly use a facemask. Such high regularity of use is encouraging but according to some respondents, a sizable portion of respondents was either buying the facemasks on their own or using one for a prolonged time. This is unsustainable and the risk of infection is high because of the repetitive use of the same PPE without appropriate cleaning or sterilization. Shortage of PPE is not a unique situation to the current survey site; similar observations have been reported from other low- and lower middle-income countries (13, 21, 22).
Limitations
The cross-sectional nature of the survey limits assertions about the cause and effect relationship. The data presented in this survey are self-reported and partly dependent on the participants’ honesty and ability to recall. Besides, COVID-19 is very dynamic, and therefore, what held during the data collection period may not be the case at a later time. Despite these limitations, our findings provide a valuable insight into the knowledge, risk perception, and practice of preventive measures of HCWs and support staff during the survey period.
Conclusions and recommendation
It is encouraging that the majority of HCWs at the SPHMMC Hospital tried their best to equip themselves with knowledge about COVID-19. The self-reported practice of IPC measures appeared to be frequent by HCWs, particularly those in service at the hospital for a long time. However, the current survey particularly identified that allied HCWs and support staff appear to lack some fundamental knowledge about the prevention of the disease, and this might be a real concern and requires prompt intervention through additional campaigns of hands-on training, health education, and drafting of local IPC guidelines. Such campaigns would be beneficial if organized based on individual circumstances (profession, level of understanding, and gender). Furthermore, there is a widely shared concern about the lack of PPE and separate public transportation, and this ought to be addressed as much as resources allow.
Acknowledgments
We acknowledge the HCWs and support staff of SPHMMC for actively participating in this survey and sharing their experiences. We are also grateful to the data collectors.
References
- Yin Y, Wunderink RG. MERS, SARS and other coronaviruses as causes of pneumonia. Respirology 2018; 23: 130–7. doi: 10.1111/resp.13196
- Zhou W. The coronavirus prevention handbook: 101 based tips that could save your life. New York, NY: Skyhorse Publishing; 2020.
- Eurosurveillance Editorial Team. Note from the editors: World Health Organization declares novel coronavirus (2019-nCoV) sixth public health emergency of international concern. Euro Surveill 2020; 25: 2019–20. doi: 10.2807/1560-7917.ES.2020.25.5.200131e
- Sohrabi C, Alsafi Z, O’Neill N, Khan M, Kerwan A, Al-Jabir A, et al. World Health Organization declares global emergency: A review of the 2019 novel coronavirus (COVID-19). Int J Surg 2020; 76: 71–6. doi: 10.1016/j.ijsu.2020.02.034
- Worldometer. Coronavirus update (live): Cases and deaths from COVID-19 virus pandemic. L’Aquila: Department of Life, Health and Environmental Science, University of L’Aquila, Worldometers; 2021.
- Zhou P, Huang Z, Xiao Y, Huang X, Fan XG. Protecting Chinese healthcare workers while combatting the 2019 novel coronavirus. Infect Control Hosp Epidemiol 2020; 41: 745–6. doi: 10.1017/ice.2020.60
- Erdem H, Lucey DR. Healthcare worker infections and deaths due to COVID-19: A survey from 37 nations and a call for WHO to post national data on their website. Int J Infect Dis 2021; 102: 239–41. doi: 10.1016/j.ijid.2020.10.064
- Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA 2020; 323: 1061–9. doi: 10.1001/jama.2020.1585
- Lu D, Wang H, Yu R, Yang H, Zhao Y. Integrated infection control startegy to minimize nosocomial infection of coronavirus disease 2019 among ENT healthcare workers. J Hosp Infect 2020; 104: 454–5. doi: 10.1016/j.jhin.2020.02.018
- Bhagavathula AS, Aldhaleei WA, Rahmani J, Mahabadi MA, Bandari DK. Novel coronavirus (COVID-19) knowledge and perceptions: A survey on healthcare workers. JMIR Public Health Surveill 2020; 6: e19160. doi: 10.2196/19160
- SPHMMC. St. Paul’s Hospital Millennium Medical College at a glance. St. Paul’s Hospital Millennium Medical College; 2020. Available from: https://sphmmc.edu.et/about/ [cited 12 April 2020].
- Olum R, Chekwech G, Wekha G, Nassozi DR, Bongomin F. Coronavirus disease-2019: Knowledge, attitude, and practices of health care workers at Makerere University Teaching Hospitals, Uganda. Front Public Health 2020; 8: 1–9. doi: 10.3389/fpubh.2020.00181
- Wang J, Zhou M, Liu F. Reasons for healthcare workers becoming infected with novel coronavirus disease 2019 (COVID-19) in China. J Hosp Infect 2020; 105: 100–1. doi: 10.1016/j.jhin.2020.03.002
- Clements JM. Knowledge and behaviors toward COVID-19 among US residents during the early days of the pandemic. JMIR Public Health Surveill 2020; 6: e19161. doi: 10.2196/19161
- Zhong BL, Luo W, Li HM, Zhang Q-Q, Liu X-G, Li W-T, et al. Knowledge, attitudes, and practices towards COVID-19 among chinese residents during the rapid rise period of the COVID-19 outbreak: A quick online cross-sectional survey. Int J Biol Sci 2020; 16: 1745–52. doi: 10.7150/ijbs.45221
- Giao H, Han NTN, Van Khanh T, Ngan VK, Van Tam V, Le An P. Knowledge and attitude toward COVID-19 among healthcare workers at District 2 Hospital, Ho Chi Minh City. Asian Pac J Trop Med 2020; 13: 260–5. doi: 10.4103/1995-7645.280396
- Gerhold L. COVID-19: Risk perception and coping strategies. PsyArXiv; 2020. Available from: https://psyarxiv.com/xmpk4/ (preprint) [cited 23 September 2020].
- Zhang M, Zhou M, Tang F, Wang Y, Nie H, Zhang L, et al. Knowledge, attitude, and practice regarding COVID-19 among healthcare workers in Henan, China. J Hosp Infect 2020; 105: 183–7. doi: 10.1016/j.jhin.2020.04.012.
- Maleki S, Najafi F, Farhadi K, Fakhri M, Hosseini F, Naderi M. Knowledge, attitude and behavior of health care workers in the prevention of COVID-19. Research Square; 2020. Available from: https://doi.org/10.21203/rs.3.rs-23113/v1 (preprint) [cited 25 April 2020].
- Alfahan A, Alhabib S, Abdulmajeed I, Rahman S, Bamuhair S. In the era of corona virus: Health care professionals’ knowledge, attitudes, and practice of hand hygiene in Saudi primary care centers: A cross-sectional study. J Community Hosp Intern Med Perspect 2016; 6: 32151. doi: 10.3402/jchimp.v6.32151
- Shoman H, Karafillakis E, Rawaf S. The link between the West African ebola outbreak and health systems in Guinea, Liberia and Sierra Leone: A systematic review. Global Health 2017; 13: 1–22. doi: 10.1186/s12992-016-0224-2
- Raab M, Pfadenhauer LM, Millimouno TJ, Hoelscher M, Froeschl G. Knowledge, attitudes and practices towards viral haemorrhagic fevers amongst healthcare workers in urban and rural public healthcare facilities in the N’zérékoré prefecture, Guinea: A cross-sectional study. BMC Publ Health 2020; 20: 1–8.