PRACTICE FORUM
Challenges faced in the conversion of a tertiary healthcare centre into a COVID-19 hospital and developing a free-standing isolation centre in India
Brajesh Kumar Ratre1, Balbir Kumar2*, Rakesh Garg1, Saurabh Vig2, Anuja Pandit2, Shweta Arun Bhopale2 and Sushma Bhatnagar1
1Department of Onco-Anaesthesia & Palliative Medicine, Institute Rotary Cancer Hospital (IRCH), All India Institute of Medical Sciences (AIIMS), New Delhi, India; 2Department of Onco-Anaesthesia & Palliative Medicine, National Cancer institute (NCI) Jhajjar, All India Institute of Medical Sciences (AIIMS), New Delhi, India
Abstract
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) causes coronavirus disease 2019 (COVID-19), which is a highly virulent disease associated with high mortality. Its outbreak into a pandemic has challenged the healthcare system of most countries around the world. A large number of infectious diseases hospitals are the need of hour to counteract this worrying infection. However, it is not possible to build such hospitals on a large scale within a short period of time; the only possibility is to convert existing healthcare facilities into COVID-19 facilities. The Centers for Disease Prevention and Control (CDC) has released guidelines for the preparation of COVID-19 hospitals, but execution at the ground level comes with many challenges. Here, we share our experience and the challenges we faced during the preparation of a tertiary healthcare centre into a COVID-19 centre, with the hope that it will help other institutions to prepare.
Keywords: COVID-19; pandemic; hospital; healthcare systems; isolation hospitals; India
Citation: Int J Infect Control 2022, 18: 20476 – http://dx.doi.org/10.3396/ijic.v18.20476
Copyright: © 2022 Rakesh Garg et al. This is an Open Access article distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for any purpose, even commercially, provided the original work is properly cited and states its license.
Received: 21 June 2020; Accepted: 19 February 2021; Published: 16 February 2022
Competing interests and funding: The authors declare no conflict of interest. The authors have not received any funding or benefits from industry or elsewhere to conduct this study.
*Balbir Kumar, Department of Onco-Anaesthesia & Palliative Medicine, National Cancer Institute, All India Institute of Medical Sciences, New Delhi, India. Email: dr.Baalbir10@gmail.com
The recent outbreak of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which is responsible for the coronavirus disease 2019 (COVID-19), started in Wuhan, China, on 31 December 2019 (1). It rapidly became a pandemic within a short span of time and spread over 210 countries/territories, and the World Health Organization (WHO) declared it as a global health emergency (2). Like other countries, it penetrated India with the first case reported on 30 January 2020, and then started evolving at an alarming rate and became an epidemic. The management of COVID-19 not only requires trained manpower but also the presence of appropriate healthcare facilities to manage this virulent disease. Being an infectious disease care facility, the healthcare facility has specific requisites such as construction of a new infectious disease hospital or conversion of an existing healthcare facility into an infectious disease hospital (3). COVID-19 patients are at significantly high risk of developing severe respiratory symptoms, including respiratory failure and the need for critical care setup. Given the limited availability of infectious disease hospitals, there was a dire need for an isolation centre and healthcare facility for the management of COVID-19 patients. In this scenario, the most appropriate way is to convert the existing healthcare facility to a COVID-19 facility, rather than building a new infrastructure which is very difficult to achieve within a short period of time. In developing countries like India with limited financial resources, converting an already established tertiary healthcare centre into a COVID-19 hospital still presents many hurdles. Here, we would like to share our experience of developing an existing healthcare facility into a COVID-19 centre including a freestanding isolation centre. Having both a freestanding isolation centre and a COVID-19 hospital is desirable, and patients may be admitted to either one based on the severity of disease. The freestanding isolation centres attached to a COVID-19 hospital allow institutionalisation of more patients for better care.
Infrastructure modification
Healthcare facilities usually care for patients with different diseases of variable severity. If a healthcare facility continues to provide care to non-COVID-19 patients and COVID-19 patients, a strict infection control protocol is needed to avoid cross-contamination between different categories of patients and healthcare workers (HCWs). Even if the healthcare facility is fully dedicated to COVID-19, triage is required to categorise the patient according to the severity of infection and any associated comorbidities. Such a facility may be labelled as a freestanding isolation facility for patients who are asymptomatic or have mild COVID-19 symptoms, and as a healthcare facility for sicker patients or with associated comorbidities like diabetes, hypertension, cardiac disease, etc.). The design and structure of isolation areas and COVID-19 treatment areas play a very important role.
Freestanding isolation facility
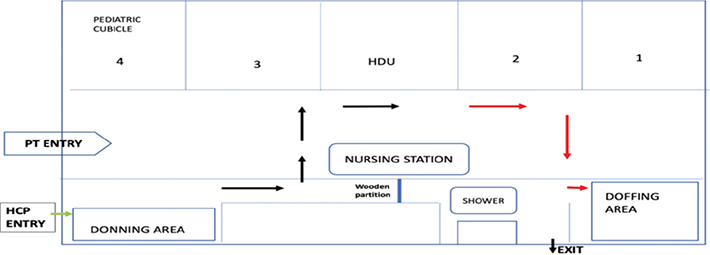
The freestanding isolation facility is helpful since not all patients require complex medical care; for these patients, isolation and basic care is desirable. Such facilities should have the appropriate infrastructure and manpower to provide this care and to identify when patients become sicker and need more advanced care. These facilities may be associated with a nearby hospital for shifting of the patient if the need arises. The isolation area for COVID-19 patients should have separate, well-ventilated rooms with attached bathrooms for individual patient. Infrastructure must include a separate facility for the donning and doffing of personnel protective equipment (PPE) by HCWs. The location of these areas should be chosen, so that HCWs do not contaminate the clean area whilst they are donning. The clean and soiled areas should have a physical barrier between the two with a one-way entry and exit. For our COVID-19 centre, we modified a residential complex near the hospital into an isolation area because it is a well-ventilated 13-floor building with single rooms and attached washrooms. The layout was modified as per the isolation need of COVID-19 patients (Fig. 1). To prevent cross-contamination, we followed the Centers for Disease Prevention and Control (CDC) guideline (4). There were separate entries and exits for HCWs and patients. HCWs enter the facility from the main gate of the building and use different routes (stairs in our case) to reach the clean area on the first floor; then, they don properly and proceed to the patient screening area. Patients enter the building through a separate route (emergency gate) at the other side of the building to reach the screening area. This arrangement allows separate entry and exit of HCWs and patients.
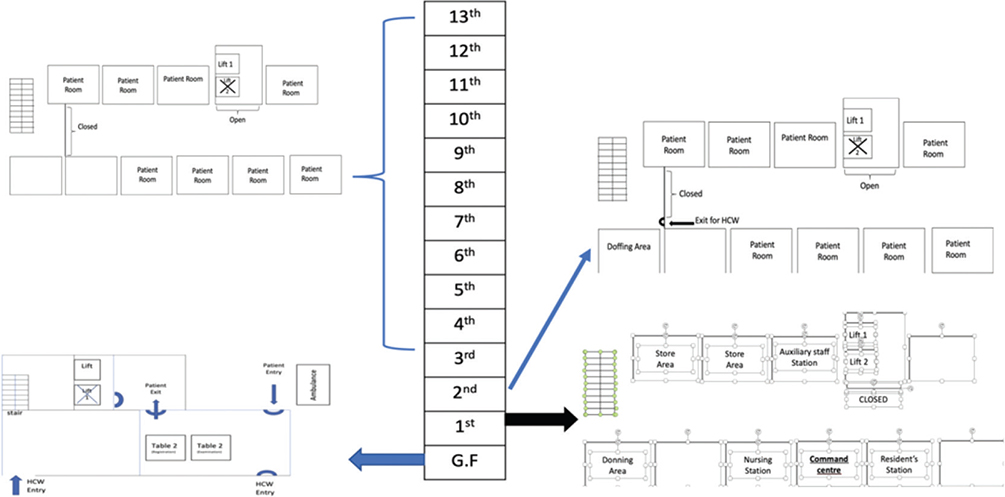
Fig. 1. Layout of free-standing isolation facility showing modifications.
HCW – healthcare worker; GF – ground floor.
Screening area
The screening area was prepared on the ground floor of the building (free-standing isolation facility) where we arranged two chairs for HCWs on one side of the table (2.5 m wide × 6 m long) with the patient sitting on the chair across the table. A glass partition was created just above the table to separate the patient from HCWs. One desktop computer was also arranged in the screening area for the registration and creation of patient hospital identity to minimise paperwork. Once the patients were screened, they were shifted by hospital staff to the allotted room via the lift available in that area (soiled), which opens from the second floor onwards, as the first-floor area was designated as a clean area. After screening, HCWs also used the same lift in the soiled area to reach the second floor onwards to review and manage patients for any further advice. The doffing area also included a bathing area in the direction of soiled to clean area. After doffing and bathing, HCWs exited from the clean area via stairs.
Donning and doffing areas
Donning and doffing are the most important steps in the management of COVID-19 patients because any carelessness or loophole in the process may lead to direct exposure of a HCW to COVID-19 infection. To avoid this, we provided a buddy in both areas to help with the procedure and to check that all steps were carried out correctly. Moreover, in the donning and doffing areas, we pasted the stepwise flowchart for donning and doffing (Fig. 2a and 2b), so that HCWs would not make any mistake during either procedure. Full height mirrors were also fixed to the opposite wall to self-check the appropriateness of donning.
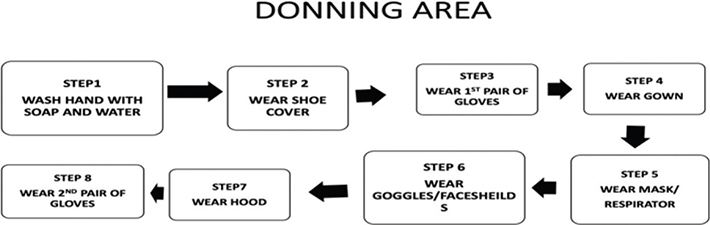
Fig. 2. (a) Flow chart of donning steps.
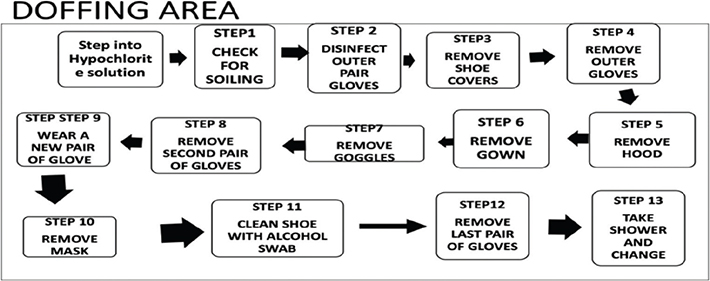
Fig. 2. (b) Flow chart of donning steps.
Hospital-based COVID-19 facility
The hospital-based facility included both the ward and the intensive care unit (ICU). Admission to the ward or ICU was based on the severity of the COVID-19 patients.
COVID-19 ward
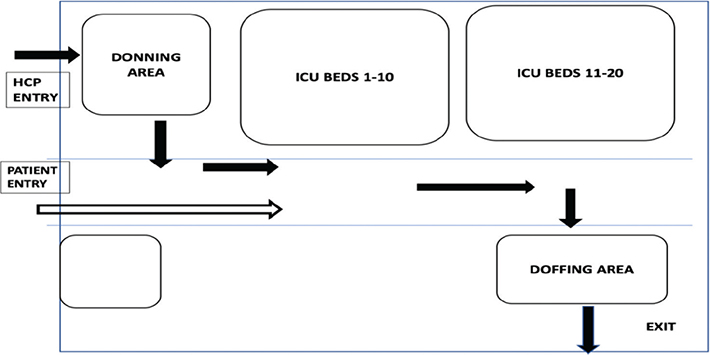
Patients who were sicker, needed oxygen or required monitoring were shifted to the isolated facility of the COVID-19 ward. Patients being shifted to the COVID-19 ward entered separately from the main gate of the hospital, with the ambulance directly dropping the patient close to a separate lift that opens directly onto the designated COVID-19 ward. HCWs entered through a separate route with a dedicated lift. The layout of COVID-19 wards allowed separate clean and soiled areas with one-way entry to prevent cross-contamination (Fig. 3). The ward was modified to isolate the entry and exit of HCWs and patients. The donning and doffing areas were located at the entry and exit areas, respectively. This required makeshift arrangements with wooden partitions, and a shower area was set up close to the doffing area.
ICU
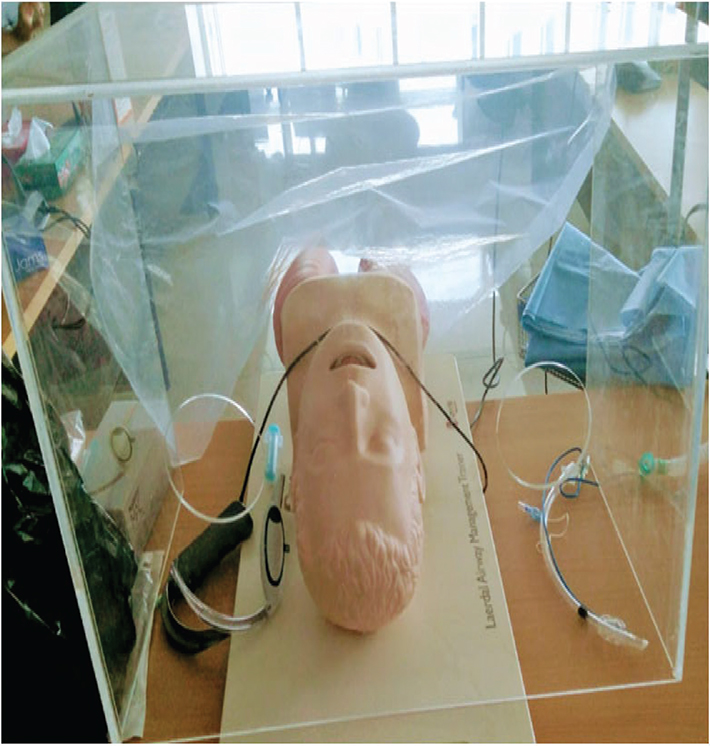
In addition to the COVID-19 ward, a 25-bed ICU was similarly prepared for critically ill COVID-19 patients (Fig. 4) who required mechanical ventilation and intensive monitoring. ICU was provided with separate donning and doffing facilities, separate patient entry, ventilators for each bed, advanced monitoring and infusion pumps, and adopted an advanced, well-integrated system for paperless monitoring of patients in critical care. We also kept an aerosol-preventing intubation box (Fig. 5) and a video-laryngoscope ready to intubate the patient.
Teaching and training of manpower
To keep the duty hours short (four shifts of 5–6 h in a day), we needed increased manpower, so a large number of HCWs from different departments of the institution were arranged to perform duties. All HCWs were trained appropriately by lecture and video demonstration on the use of PPE, such as donning and doffing, the dos and don’ts during patient care, the importance of maintaining clean and soiled areas, proper handwashing before and taking shower after doffing, and performed many mock drill exercises to enhance the performance of HCWs. The teaching and sensitisation sessions were conducted by the infection control team when HCWs were assigned to COVID-19 duties. Videos were also prepared and shared with them. Two separate sets of teams were then formed and posted to the freestanding isolation area, and the COVID-19 ward and ICU. Resident doctors from non-clinical or paraclinical departments were assigned to the isolation facility, and residents from clinical departments were asked to join the teams providing services to the COVID-19 ward and ICU. Also, as per the CDC guideline (4), our hospital suspended elective surgeries, outdoor patient visitors and routine diagnostic procedures, and also restricted the entry of visitors to the hospital to reduce facility risk.
Protocol and standard operating procedures
Specialists from the Departments of Anaesthesia, Medicine, Critical Care and Pulmonary Medicine became leaders to guide HCWs on workflow, to organise duty rosters and to form various standard operating procedures (SOPs) and protocols for patient care and treatment according to the CDC guideline (5) after conducting drill exercises with HCWs. The hospital administration department also played a significant role in the execution of plans on ground; they arranged transportation for HCWs, patients, food for HCWs and provided other logistic support. In addition, they organised meetings with higher authorities of institutions and government officials and provided any updates to working teams.
Documentation
Documentation is very important for patient management and record keeping. However, excessive paperwork can be a source of infection if brought into a clean area from an infected COVID-19 area. To minimise the possibility of infection from this source, all patient-related information was recorded electronically. This required usage of computers with internet connection to be installed in COVID-19 areas and usage of tablets on clinical rounds. In the screening area, patient details were entered along with a focused history and report status, and the desktop computer generated a one page (face sheet) to capture this information. The face sheet was kept outside the patient room, with daily notes added to the sheet. Photographed images of the face sheet were sent via email for compiling of all data into an excel sheet on a desktop computer in the clean area. In the COVID-19 ward, we used a single ICU sheet to document clinical notes and treatment plans and maintained an excel sheet on a desktop computer as well. The ICU ward integrated an advanced, paperless real-time monitoring system. The main advantage of the paperless integrated system was real-time monitoring of patients, with this monitoring being accessible outside of the ICU by experts who could provide a valuable advice to HCWs inside the ICU, without having to go inside the ICU and, thus, reducing the risk of exposure.
Patient interaction and communication
Dissemination of information and communication was a big problem because the HCWs on duty in the isolation area and the COVID-19 ward were required to be properly donned, meaning they were unable to move out to call for help. To overcome this, we installed a command centre in another building equipped with Skype (Microsoft Corporation, Washington, USA) on a desktop computer and an intercom connection, so that senior faculty could monitor the situation and give valuable advice to working teams in both places. It reduced the risk of exposure by minimising visits to patient areas. Also, one smart phone was provided to the resident doctor in a clean area of isolation, where patients could directly make a video call if facing any problem to save time and reduce the risk of repeated exposure. All patients were provided a Whatsapp (Facebook, Inc., California, USA) mobile number so that video chatting could be done from either end for any query or assistance.
Transportation
The transportation of COVID-19 patients from one place to another should be for a particular reason such as patient treatment or diagnostic intervention. CDC has issued a clear guideline for the transportation of patients, which we followed, but we faced the challenge of a 1-km distance between the isolation area and the COVID-19 ward. This meant it took a long time to transfer any patients who became sicker or collapsed in the isolation area to the COVID-19 ward and could adversely affect outcomes if not managed well during transportation. To overcome this, we kept one crash cart with all emergency drugs, intubation cart and trolley ready on the ground floor for quick action and had one fully equipped advanced ambulance at the isolation area for immediately shifting the patient to the ward.
Psychological stress and burnout of HCWs
Another obstacle was the psychological stress and fear amongst the HCWs. HCWs were under high stress from multiple factors including anxiety over the lethality of infection, concern for their family wellbeing and, predominantly, from any news of HCWs getting an infection due to COVID-19 and increased workloads because of strict infection control measures. To counter this, we arranged regular meetings with HCWs and updated them on the current situation through various modes of communication, and we provided a balanced diet under the supervision of a dietician. Also, in the evening, we arranged light music and singing after duty hours to raise morale whilst keeping in mind social distancing. The help of a psychologist was enlisted for HCWs needing further support.
Clinical management
No definitive, curative treatment has been currently approved for COVID-19 patients. Mild symptomatic patients may not initially require hospitalisation, but the decision to monitor the patient in an inpatient or outpatient setting should be made on a case-to-case basis. Severely ill patients require hospitalisation because of complications like pneumonia, acute respiratory distress syndrome (ARDS), sepsis, etc. Such patients may need tracheal intubation and ventilatory support, which are associated with many of the issues described below.
Airway management and ventilatory support
The risk of transmission of infection is very high in HCWs associated with the tracheal intubation of critically ill patients because of the highly aerosol-generating procedure with a high level of viral shedding in very sick patients. To prevent transmission, as per the guideline of Surviving Sepsis Campaign (SSC) (6) by the European Society of Intensive Care (ESICM) and the Society of Critical Care Medicine (SCCM), we made sure that tracheal intubation was performed by the most experienced person of the team using video-laryngoscope to reduce the number of attempts. Also, we prepared a plastic transparent intubation box (Fig. 5) along with a transparent plastic cover, so that the head end of the patient was covered but remained visible during tracheal intubation to avoid direct exposure to aerosol during intubation.
Conclusion
During the transformation of a tertiary care centre into a COVID-19 hospital, we faced various problems, including infrastructure changes to set up the isolation area, ward and ICU; infection control; manpower arrangement and their transition into organised teams; communication and transportation of patients; psychological well-being of HCWs; and airway management of sick patients. To overcome these various issues, we adopted stepwise, well-organised approaches.
Ethical approval
Ethics approval was not required.
References
- Wu JT, Leung K, Leung GM. Nowcasting and forecasting the potential domestic and international spread of the 2019-nCoV outbreak originating in Wuhan, China: a modelling study. Lancet 2020; 395(10225): 689–97. doi: 10.1016/S0140-6736(20)30260-9
- World Health Organization. Statement on the second meeting of the International Health Regulations (2005) Emergency Committee regarding the outbreak of novel coronavirus (COVID-2019). Available from: https://www.who.int/news-room/detail/30-01-2020-statement-on-the-second-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-outbreak-of-novel-coronavirus-(2019-ncov) [cited 28 February 2020].
- Liu Y, Li J, Feng Y. Critical care response to a hospital outbreak of the 2019- nCoV infection in Shenzhen, China. Crit Care 2020; 24(1): 56. doi: 10.1186/s13054-020-2786-x
- Available from: https://www.cdc.gov/coronavirus/2019-ncov/infection-control/control-recommendations.html [cited 3 June 2020].
- Al-Dorzi HM, Aldawood AS, Khan R, Baharoon S, Alchin JD, Matroud AA, et al. The critical care response to a hospital outbreak of Middle East respiratory syndrome coronavirus (MERS-CoV) infection: an observational study. Ann Intensive Care. 2016 Dec;6(1):101. doi: 10.1186/s13613-016-0203-z
- Alhazzani W, Evans L, Alshamsi F, Møller MH, Ostermann M, Prescott HC, et al. Surviving sepsis campaign guidelines on the management of adults with coronavirus disease 2019 (COVID-19) in the ICU: first update. Critical care medicine. 2021 Mar 1;49(3):e219–34.