ORIGINAL ARTICLE
Self-medication practice and associated factors among adults in Wolaita Soddo town, Southern Ethiopia
Tamirat Mathewos1, Kassa Daka1, Shimelis Bitew1 and Deresse Daka2*
1Wolaita Soddo University, College of Health Sciences, School of Public Health; 2Hawassa University, College of Medicine and Health Sciences, Faculty of Medicine
Abstract
Background: Self-medication is the selection and use of medicines by individuals to treat their self-recognized illnesses or symptoms. Self-medication can decrease costs and enable health professionals to concentrate on more serious health problems.
Aim: To assess self-medication practice and associated factors among adults in Wolaita Soddo town, Southern Ethiopia, 2017.
Methods: An institution-based cross-sectional study was conducted from September 30 to October 30, 2017. A multi-stage sampling technique of drug retail outlets in Wolaita Soddo town was employed to identify 623 individuals that came to buy drugs in the past three months. Data was collected using a structured questionnaire.
Results: About 33.7% of the respondents had practiced self-medication in the past 3 months. Multivariate analysis revealed that female sex (adjusted odds ratio (AOR) = 2.22, 95% confidence interval (CI): 1.47–3.36), low income (AOR = 3.95, 95% CI: 2.32–6.73) and higher educational level (AOR = 5.79, 95% CI: 2.47–13.58) were the independent factors significantly affecting the practice of self-medication with drugs. Headache/fever (32.4%), respiratory tract infections (31.4%) and gastrointestinal diseases (16.2%) were the most frequently reported illnesses or symptoms of illnesses that prompted self-medication of study participants.
Conclusion: Health education campaigns, strict legislations on dispensing drugs from private pharmacies, and improving accessibility and affordability of health care are among the important interventions required to change people’s health-seeking behavior and prevent the potential risks of self-medication.
Keywords: Self-medication; drug retail outlets; over-the-counter; prescription; Ethiopa.
Citation: Int J Infect Control 2021, 17: 20322 – http://dx.doi.org/10.3396/ijic.v17.20322
Copyright: © 2021 Tamirat Mathewos et al. This is an Open Access article distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), allowing third parties to copy and redistribute the material in any medium or format and to remix, transform, and build upon the material for any purpose, even commercially, provided the original work is properly cited and states its license.
Received: 7 May 2020; Accepted: 31 May 2020; Published: 27 May 2021
Competing interests and funding: The authors declare that they have no competing interests.
The study was supported by Wolaita Soddo University. The support included payment for data collectors and purchase of materials and supplies required for the study. The support did not include designing of the study, analysis, and interpretation of data and manuscript preparation.
*Deresse Daka, Hawassa University. Email: drsdk200@gmail.com
The World Health Organization (WHO) defines self-medication as the selection and use of medicines by individuals to treat self-recognized illnesses or symptoms (1). It is an element of self-care in which people utilize traditional or modern medicine without consulting a physician, either for diagnosis, prescription or surveillance of treatment. Self-medication comprises obtaining medicines without authorized prescription, resubmitting old prescriptions to buy medicines, using medicines in share with relatives or social life members, or utilizing leftover medicines stored at home (2).
Self medication is practiced commonly in the world in both developed and developing countries, and its utilization may be even more than prescribed medication (3). The prevalence of self-medication practice (SMP) was found to be: Pakistan 85% (4, 5), Saudi Arabia 35.4% (3), Iran 53% (6), Yemeni 85% (7), India 92.8% (8); Brazil 16.1%, (9) Latin American immigrants in Seville, Spain 77.4% (10), Italy 69.2% (11), Greece 54.7% (12) and Spain 20.2% (13); Nigeria 95% – 98%, Southwestern Nigeria, 81.8% (16), and Kenya 76.9% (17).
A study conducted in Addis Ababa showed that the magnitude of SMP was 50% (18), with other studies showing the following prevalence of SMP in Ethiopia: Kolladiba town, Northwest Ethiopia 62.8% (19), Assendabo town, Southwestern Ethiopia 39.2% (20), Sire town, West Ethiopia 27.16%,2 and the Silte zone, South Ethiopia 24.4% (21). Another study conducted at Gondar University showed that 38.5% of the participants practiced self-medication (22).
According to a study conducted in South Karnataka, India, the most common symptoms prompting self-medication were: gastric symptoms (72.10%), joint pain (65.89%), headache (63.02%), fever (47.87%), and common cold (37.95%) (23).The study also showed that the main groups of diseases in which patients self-medicated were respiratory diseases (39.9%), common cold (39.5%) and headache (37.3%) (6).
In a study conducted in Mekelle town to assess SMP, the most frequent illnesses or symptoms of illnesses that prompted study participants to self-medicate were headache/fever (20.7%), gastrointestinal diseases (17.3%) and respiratory tract infections (15.9%) (24). In Addis Ababa, commonly reported illnesses or symptoms of illnesses for which respondents self-medicated were gastrointestinal (25.1%), headache/fever (24.9%) and respiratory problems (21.4%) (18).
In a study conducted on self-medication practices in Italy, non-steroidal anti-inflammatory drugs (NSAIDS) (83.5%) were most commonly used, whereas antibiotics (26.7%), antacids (4.2%), and corticosteroids (3.4%) have been used less frequently (11).Another study on SMP among Iraqi patients in Baghdad city showed that antibiotics (74.7%) were the most frequently requested drugs followed by paracetamol (55.1%), antihistamines (36.2%), and NSAIDS (27%) (25).
A study conducted on self-medication in Alexandria, Egypt, showed that analgesics (96.7%), cough and common cold preparations (81.9%), vitamins and minerals (63.2%), antibiotics (53.9%), gastrointestinal drugs (51.4%), and antihypertensives (16.1%) were the most commonly used drugs in self-medication by participants (26).
In a study conducted on SMP in Addis Ababa, the most common types of drugs were analgesics/antipyretics (33.1%), antimicrobials (26.4%) and gastrointestinal drugs (17.7%) (18).A study on SMP in Jimma town, Ethiopia, indicated that the most common drugs used for self-medication were analgesics/antipyretics (28.94%), antimicrobials (28.13%) and antihelmintics (17.56%) (27).
A cross-sectional study conducted on prevalence and pattern of SMP in an urban area of Delhi, India showed that the major sources of information for self-medication were past experience (46.5%) followed by a physician’s old prescription (43.8%), recommendation by chemists (35.6%) and family members’ opinion (35.6%) (8). Similarly in Alexandria, Egypt, the most common source of advice or information about self-medication with drugs was an old prescription (73.9%), pharmacists (42.7%), and an older person in the household or friend (30.5%) (26).
A study conducted in Addis Ababa showed that 39% of drug consumers received advice from health professionals like physicians, nurses and health assistants but without formal prescriptions. About 23.5% of participants were advised by friends, relatives or neighbors, who themselves had no background in the health profession. Pharmacists or other personnel working in pharmacies were found to be sources of advice for 15.4% of respondents, whereas 20% of respondents received no advice but had information on the drugs from labels, leaflets or promotional materials (18).
Studies conducted in different countries have shown that age, sex, poor health status, inconvenient access or services (3), along with education (9), place of residence, marital status, occupation, old age group (6), and presence of chronic diseases (26), were factors for self-medication. Convenience of pharmacy, friend/peer pressure and advertisements (28), unavailability of physicians, prior experience treating the same illness and requirement of emergency care were other factors for self-medication (29).
In a study on self-medication practice in Mekelle, Ethiopia, the main reasons for self-medication were belief that the illness is mild (21.7%), previous experience of illness/ medicine (20.7%), inexpensive and time-saving (20.2%), belief that it was an emergency situation (17%), and prevention of known or unknown illness (16.9%) (24).
Studies indicate that self-medication is the first response to illness among people with low income (30). A study conducted in Addis Ababa indicated that the most common reasons for self-medication were non-seriousness of illness (36.6%), emergency situations (19.8%), prior experience (18.2%), and less expensive in terms of time and money (12.6%) (18).
Methods
Study setting and population
This study was conducted in Wolaita Soddo town, 327 km from the capital city of Addis Ababa. Wolaita Soddo town has an estimated population of 140,105 number. It has 30 drug retail outlets (DROs), two hospitals, three health centers, 11 health posts and 21 private health institutions that provide health services to the community.
Study design
An institution-based cross-sectional study was conducted in nine DROs from September 30 to October 30, 2017 in the Wolaita zone of Soddo town.
Study population
All adult people >18 years of age who attend DROs to buy drugs.
Inclusion criteria
Adults (age >18 years) who buy drugs with or without a prescription from the selected DROs in Wolaita Soddo town during the study period.
Exclusion criteria
People who were not able or willing to sign informed consent.
Sample size determination
The sample size was calculated using single population proportion formula.
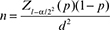
where n: sample size; p: estimated prevalence of self-medication; Z: percentile of standard normal distribution corresponding to 95% confidence level; d: the margin of error which is 0.05. By using the anticipated population proportion of 24.4% from a previous study (21), the sample size calculated as
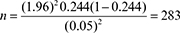
Hence, the design effect of the study was 2 and the sample become 566. The total sample size when 10% non-response was added became 623.
Sampling procedure
A multistage sampling technique was conducted to select study participants. All types of drug retail outlet such as pharmacies, drug stores and drug vendors were used. About 9 drug retail outlets were selected randomly from the total drug retail outlet and then individuals were selected systematically.
Data collection and Analysis procedure
A face to face interview was conducted with individuals coming to selected pharmacies to buy drugs during the data collection period. After gaining informed consent from the participant, background information and possible factors were collected.
Data collection tool
A pre-structured questionnaire was developed and translated into the local language, Amharic. To ensure consistency, it was then retranslated to English.
Data Quality control
Four health professionals who had previous experience on data collection were selected and trained for one day. The questionnaire was pre-tested on 5% of the actual sample size before data collection. The data was checked for completeness and consistency. The Hosmer and Lemeshow test for Goodness-of-fit of the model was done (p = 0.698).
Data processing and analysis
Data was coded and entered into the computer with EPI-data version 3.1 and exported to SPSS version 20 for analysis. Descriptive statistics such as frequencies, percentage and tables were used to present the respondent’s result. Independent variables with p < 0.25 on bivariate analysis became a candidate for multivariable analysis. Univariate and multivariate logistic regression was fitted to identify associated factors with 95% CI using p-value < 0.05.
Results
Socio-demographic characteristics
Out of the 623 individuals who participated in this study, 319 (51.2%) were males, 243 (39%) were aged 25–34 years, 404 (64.9%) were Wolaita ethnicity group, 367 (58.9%) had graduated from college or University, 351 (56.3%) were Protestant in their religion and 328 (52.6%) were married (Table 1).
| Variables | Frequency (N) | Percentage (%) |
| Sex Male Female |
319 304 |
51.2 48.8 |
| Age 18–24 25–34 35–44 >44 |
159 243 143 78 |
25.5 39 23 12.5 |
| Religion
Protestant Orthodox Muslim Othersa |
351 205 56 11 |
56.3 32.9 9 1.8 |
| Ethnicity Wolaita Amhara Gurage Oromo Gamo Othersb |
404 66 52 41 33 27 |
64.9 10.6 8.3 6.6 5.3 4.3 |
| Educational status No formal education Primary education Secondary education Higher education |
45 66 145 367 |
7.2 10.6 23.3 58.9 |
| Marital status Married Not married Widowed Divorced |
328 242 19 34 |
52.6 38.8 3.1 5.5 |
| Income (in Ethiopian Birr)d 0–500 501–1000 1001–1500 1501–2000 2001–3000 ≥3001 |
141 98 55 55 52 222 |
22.6 15.7 8.8 8.8 8.4 35.7 |
| aCatholic and pagan; bHadya, Kambata, and Sidama; cprivate employee and daily laborer; d1 USD = 27 ETB. | ||
Self-medication practice
In this study, the prevalence of SMP was 210 (33.7%) (95% CI: 37.2, 44.9). The most frequent illnesses reported by respondents that prompted them to self-medicate were headache 68 (32.4%), cough/common cold 66 (31.4%), gastrointestinal disease 34 (16.2%) and malaria 32(15.2%) (Table 2).
| Illness/symptom | Frequency (N) | Percentage (%)# |
| Fever | 23 | 11 |
| Headache | 68 | 32.4 |
| Diarrhea | 13 | 6.2 |
| Cough/common cold | 66 | 31.4 |
| Gastrointestinal disorder | 34 | 16.2 |
| Menstrual problem | 12 | 5.7 |
| Back pain | 18 | 8.6 |
| Eye infection | 10 | 4.8 |
| Skin infection | 13 | 6.2 |
| Malaria | 32 | 15.2 |
| Peptic ulcer disease | 15 | 7.1 |
| Others(typhoid and acne) | 08 | 3.8 |
| #Numbers do not add to 100% as patients might have more than one answer. | ||
Source of advice and way of requesting drugs
The most frequent source of advice for self-medication in the present study were pharmacists 117 (55.7%), other healthcare providers such as nurses and health assistants 41 (19.5%) and friends 34 (16.2%). Drug consumers were also asked how they requested the drugs they used. About 101 (48.1%) of drug consumers made their requests by relating the symptoms of their illness to a pharmacy professional, 82 (39%) of them by telling the specific name of drug, whereas 22 (10.5%) mentioned the class to which the drug belongs. Nevertheless, 2.4% of respondents requested the drug by showing an old sample of the drug or drug products (Table 3).
Reasons for self-medication
About 165 (26.5%) of the study participants believed that the disease was mild. However, 164 (26.3%) of the participants opinion was inexpensiveness and 95 (15.2%) to save their time (Table 4).
The most frequent types of drugs used for self-medication in this study were analgesics/antipyretics 118 (56.2%), antibiotics 84 (40%), and antimalarials 34 (16.2%) (Table 5).
| Drug type | Frequency (N) | Percentage (%)# |
| Analgesics/antipyretics | 118 | 56.2 |
| Antibiotics | 84 | 40 |
| Drugs for respiratory disease | 03 | 1.4 |
| Antihelmithes | 14 | 6.7 |
| Drugs for PUD | 15 | 7.1 |
| Antimalarials | 34 | 16.2 |
| Drugs for eye disease | 10 | 4.8 |
| Drugs for skin disease | 13 | 6.2 |
| Others (antiemetic and laxatives) | 09 | 4.3 |
| # Numbers do not add to 100% as patients might have used more than one drug type. | ||
Factors associated with self-medication practice
The multivariable logistic regression model showed that sex, educational status and income were statistically associated with self-medication practice. Female respondents were about twice more likely to practice self-medication than males (AOR=2.22, 95% CI: 1.47–3.36) (p < 0.05). Respondents with higher educational level were 5.8 times more likely to practice self-medication compared to those having no formal education (AOR = 5.79, 95% CI: 2.47–13.58) (p < 0.05). Study participants with low monthly income were found to be 4 times more likely to practice self-medication compared to those with higher income levels (AOR=3.95, 95% CI = 2.32–6.73)(p < 0.05) (Table 6).
| Respondent’s characteristics | Self-medication | COR (95% CI) | AOR (95% CI) | |
| Yes (%) | No (%) | |||
| Sex | ||||
| Male | 81 (38.6%) | 238 (57.6%) | 1 | 1 |
| Female | 129 (61.4%) | 175 (42.4%) | 2.166 (1.542–3.042)*** | 2.223 (1.472–3.355)*** |
| Age | ||||
| 18–24 | 51 (24.3%) | 108 (26.2%) | 1 | 1 |
| 25–34 | 91 (43.3%) | 152 (36.8%) | 1.268 (0.831–1.934) | 1.53 (0.88–2.659) |
| 35–44 | 49 (23.3%) | 94 (22.8%) | 1.104 (0.683–1.783) | 1.748 (0.835–3.658) |
| >44 | 19 (9%) | 59 (14.3%) | 0.682 (0.369–1.261)* | 1.235 (0.517–2.95) |
| Ethnicity | ||||
| Wolaita | 147 (70%) | 257 (62.2%) | 1.411 (0.749–2.658) | 1.123 (0.531–2.376) |
| Amhara | 13 (6.2%) | 53 (12.8%) | 0.605 (0.258–1.42)* | 0.452 (0.168–1.22) |
| Oromo | 13 (6.2%) | 28 (6.8%) | 1.145 (0.47–2.79) | 1.194 (0.424–3.361) |
| Gamo | 12 (5.7%) | 21 (5.1%) | 1.41 (0.557–3.569) | 1.525 (0.507–4.588) |
| Gurage | 10 (4.8%) | 17 (4.1%) | 1.451 (0.542–3.885) | 1.491 (0.442–5.032) |
| Others | 15 (7.1%) | 37 (9%) | 1 | 1 |
| Educational status | ||||
| No formal education | 9 (4.3%) | 36 (8.7%) | 1 | 1 |
| Primary education | 2 (1%) | 64 (15.5%) | 0.125 (0.026–0.610)** | 0.171 (0.033–0.882) |
| Secondary education | 19 (9%) | 126 (30.5%) | 0.603 (0.251–1.447) | 0.859 (0.325–2.269) |
| Higher education | 180 (85.7%) | 187 (45.3%) | 3.85 (1.803–8.221)*** | 5.786 (2.465–13.581)*** |
| Income | ||||
| 0–500 | 76 (36.2%) | 65 (15.7%) | 3.157 (2.024–4.923)*** | 3.949 (2.316–6.734)*** |
| 501–1000 | 39 (18.6%) | 59 (14.3%) | 1.785 (1.081–2.947)** | 1.87 (1.046–3.34)** |
| 1001–1500 | 12 (5.7%) | 43 (10.4%) | 0.753 (0.372–1.525) | 1.038 (0.464–2.325) |
| 1501–2000 | 14 (6.7%) | 41 (9.9%) | 0.922 (0.469–1.811) | 1.035 (0.481–2.229) |
| 2001–3000 | 9 (4.3%) | 43 (10.4%) | 0.565 (0.26–1.229)* | 0.48 (0.207–1.116) |
| ≥3001 | 60 (28.6%) | 162 (39.2%) | 1 | 1 |
| Marital status | ||||
| Married | 107 (51%) | 221 (53.5%) | 1 | 1 |
| Not married | 89 (42.4%) | 153 (37%) | 1.201 (0.848–1.703) | 1.16 (0.69–1.95) |
| Widowed | 8 (3.8%) | 11 (2.7%) | 1.502 (0.587–3.844) | 1.82 (0.606–5.469) |
| Divorced | 6 (2.9%) | 28 (6.8%) | 0.443 (0.178–1.101)* | 0.576 (0.202–1.646) |
| *P < 0.25; **P < 0.05; ***P < 0.001. COR, crude odds ratio; 95% CI, 95% confidence interval; AOR, adjusted odds ratio. |
||||
Discussion
Self-medication has an important role in the care of minor illness. It can decrease cost and enable health professionals to concentrate on more serious health problems. (3, 31) On the other hand, self-medication is a potential contributor to human pathogen resistance to antibiotics. Its potential risks include incorrect self-diagnosis, delay in medical treatment, incorrect treatment choice, severe adverse reactions, incorrect dosage, and drug dependence and abuse (32).
In the present study the prevalence of self-medication was 33.7% (95% Cl: 37.2, 42.2). This finding is in line with other studies carried out in different parts of the world such as Saudi Arabia (35.4%) (3) and South India (35.9%) (33). This result is also similar to studies carried out in different parts of Ethiopia such as Assendabo, Southwest Ethiopia (39.2%) (20) and Nekemte (36.7%) (34, 19). On the other hand, the prevalence of SMP in this study is lower than those conducted in India (92.8%),8 Sudan (81.8%) (16), Kolladiba (62.8%) (19), Pakistan (85%) (4), Karachi, Pakistan (84.8%) (5), Iran (53%) (6), Yemeni (85%) (7), Latin American immigrants (77.4%) (10) Nigeria (91.4%) (15) and Kenya (76.9%) (17). However, the current finding is greater than those of studies conducted in Brazil (16.1%) (9), Bahir Dar (23.3%) (35), Sire town (27.16%) (2) and Silte (24.4%) (21). This might be due to sociodemographic factors such as educational status, socio-economic status and living status of the study participants. Moreover, the prevalence of self-medication could not be compared across different studies due to the varying nature of definitions used, recall period considered, region selected and methodology adopted, the role of country culture, healthcare systems and the perceived role of health professionals.
Data from the present study showed that sex, income and educational status had significant association with self-medication practice. Female respondents were more likely to practice self-medication than males. This finding is consistent with studies conducted in Brazil (9), Iran (36), Italy (11), Greece (12), Serbia (37), Arsi University (38), Kolladiba (19). The fact that females have significant social roles, are more strongly self-care oriented than male and have more active involvement in household activities making them tend not to seek other medical service are other reasons for the increased practice of self-medication among females (12). However, contradicting literature showing that men self-medicate more than women were found in South Karnakata (23), and Saudi Arabia (3).
This study showed that respondents with low socio-economic status were more likely to practice self-medication compared to those with higher income, which is in line with studies conducted in Kharthoum (16) and Kolladiba (19). In the majority of economically deprived countries, nearly 60–80% of health related problems are treated through self-medication as a lower cost alternative. As WHO indicated, self-medication provides a cheap alternative to people who cannot afford to pay healthcare costs, and thus, self-medication is often the first response to illness among people with low income (20, 39). Most people prefer self-medication than going to health facilities because of high costs of laboratory diagnosis and other services.
In this study, participants with higher educational status practice self-medication higher than those with no formal education, which is consistent with previous studies conducted in Iran (36), Spain (13), Greece (12), Rajasthan (40), and India (8). Respondents with college and university educational level have more knowledge about common diseases and drugs for self-treatment than those who are less educated. Moreover, people with higher educational status have more self-confidence in self-diagnosis and self-medication, especially where there is acute illness and as a result they are capable of identifying appropriate drugs to treat their symptoms, whereas less educated people prefer a medical consultation (12).
Headache was the primary symptom for practicing self-medication in the present study, which is supported by studies conducted in Karachi (5), Pakistan (4), Mekelle (24), Kolladiba (19), Silte (21). However, this finding contradicts results from a study conducted in Addis Ababa (18), in which gastrointestinal disease was the most frequently reported illness for self-medication. In this study, cough/common cold, gastrointestinal disease and malaria were the most frequently reported illnesses following headache that necessitated self-medication, consistent with findings in Kolladiba, Ethiopia (19)
In the present study, analgesics/antipyretics were the most frequently utilized drug classes as indicated in other studies done in Brazil (9), India (41), Kolladiba (19), Mekelle (24), Jimma (27) and Southwest Ethiopia (42). This is because these drugs are used to treat mild common symptoms such as headache, fever and pain. It confirms that analgesics/antipyretics are the most commonly utilized over the counter drugs for self-medication. Similarly, antibiotics and antimalarials were frequently utilized drug classes next to analgesics in the present study, which is in line with studies conducted in Iraq (25), Jimma (27), India (41), Kolladiba (19), Southwest Ethiopia (42), Arsi University (38) and Addis Ababa (18).
In the present study, mildness of disease, inexpensiveness of self-medication, and saving time were pointed out as major reasons for self-medication, supported by studies conducted in Mekelle (24), Addis Ababa (18), Rajasthan (40), Sudan (16) and Sire town (2).
Conclusion
According to our study, self-medication is practiced for both over-the-counter and prescription only drugs. Respondents who were female, having low socio-economic status, divorced and higher educated were more likely to practice self-medication. Headache/fever, RTIs and GITs were the most frequently reported symptoms of illnesses that prompted self-medication. The major reasons for SMP were mildness of disease, inexpensiveness of self-medication and saving time. Analgesics/antipyretics, Antibiotics, and Antimalarials were the most frequently requested drug classes. Health professionals, especially community pharmacists, need to educate people on the benefits and risks of self-medication to encourage responsible self-medication. Future research to assess the practice of Self-medication should be conducted.
Declaration
Ethics approval and consent to participate
An ethical approval was obtained from the Ethical Review Committee of Wolaita Soddo University, College of Health Sciences, Research and Community Service Office. Official support letter was obtained from Wolaita Soddo University and Wolaita zone health department for undertaking the study. An informed consent was obtained from each of the study participants. Each participant took part in the study after verbal consent was approved.
Acknowledgments
The authors would like to thank Wolaita Soddo University, Wolaita Soddo City Administration and study participants.
Author’s contribution
TM: conceived and designed the study, performed the data collection, analyzed the data, KD: involved in protocol development, data analysis and manuscript write-up; SB: conceived and designed the study, data collection; DD: involved in data analysis and manuscript write up. All authors have read and approved the manuscript.
Availability of data
The raw data should not be provided in order to protect patient’s anonymity. Summary data are available in the main documents.
Consent for publication
Not applicable.
References
- World Health Organization. The Role of the pharmacist in self-care and self-medication: report of the 4th WHO Consultative Group on the Role of the Pharmacist, The Hague, The Netherlands, 26–28 August 1998. World Health Organization. Available from: https://apps.who.int/iris/handle/10665/65860.
- Jaleta A, Tesema S, Yimam B. Self-medication practice in Sire town, West Ethiopia: a cross-sectional study. Cukurova Med J 2016; 41(3): 447–52.
- Alghanim SA. Self-medication practice among patients in a public health care system. East Mediterr Health J 2011; 17(5): 409–16.
- Haseeb A, Bilal M. Prevalence of using non prescribed medications in economically deprived rural population of Pakistan. Arch Public Health 2016; 74: 1.
- Afridi MI, Rasool G, Tabassum R, Shaheen M, Siddiqullah, Shujauddin M. Prevalence and pattern of self-medication in Karachi: A community survey. Pak J Med Sci 2015; 31(5): 1241–45.
- Azami-Aghdash S, Mohseni M, Etemadi M, Royani S, Moosavi A, Nakhaee M. Prevalence and Cause of Self-Medication in Iran: A Systematic Review and Meta-Analysis Article. Iran J Public Health 2015; 44(12): 1580–93.
- Mojali S, Al-Ghanim SA, Alduais AMS, Al-Shabrani BF. Self-medication practice among Yemeni patients in Ibb city: a survey study exploring patients’ perceptives. J Hosp Admin 2015; 4(4): 32–39.
- Kumar V, Mangal A, Yadav G, Raut D, Singh S. Prevalence and pattern of self-medication practices in an urban area of Delhi, India. Med J DY Patil Univ 2015; 8(1): 16–20.
- Arrais PSD, Fernandes MEP, da Silva Dal Pizzol T, et al. Prevalence of self-medication in Brazil and associated factors. Rev Saude Publica 2016; 50(Suppl 2): 1s-11s.
- Gonzalez-Lopez JR, Rodrigez-Gazquez M and Lomas-Campos M. Self-medication in adult Latin American immigrants in Seville. Acta Paul Enferm 2012; 25(2) :75–81.
- Garofalo L, Di-Giuseppe G, Angelillo IF. Self-Medication Practices among Parents in Italy. Biomed Res Int 2015; 2015: 580650, 8 p.
- Papakosta M, Zavras D, Niakas D. Investigating factors of self-care orientation and self-medication use in a Greek rural area. Rural Remote Health 2014; 14: 2349
- Carrasco-Garrido P, Hernández-Barrera V, López de Andrés A, Jiménez-Trujillo I, Jiménez-García R. Sex-differences on self-medication in Spain. Pharmacoepidemiol Drug Saf. 2010; 19(12): 1293–99.
- Afolabi AO. Factors influencing the pattern of self-medication in an adult Nigerian population. Ann Afr Med 2008; 7(3): 120–7.
- Osemene KA, Lamikanra A. A Study of the Prevalence of Self-Medication Practice among University Students in Southwestern Nigeria. Tropical J Pharmaceutical Res 2012; 11(4): 683–9.
- Awad AI, Eltayeb IB, Capps PA. Self-medication practices in Khartoum State, Sudan. Eur J Clin Pharmacol 2006; 62(4): 317–24.
- Owour IA, Alwar J, Oyugi H. Perceptions Influencing Self Medication with Antibiotics and/or Antimalarials among the Households in Nyalenda B Sub-Location, Kisumu County, Kenya. Am J Public Health Res 2015; 3(3): 116–21.
- Tenaw A, Tsige G-M. Self-medication practices in Addis Ababa: a prospective study. Ethiop J Health Sci 2004;14(1): 1–11.
- Abrha S, Kassa FM, Melka W. Self-medication Practice: the Case of Kolladiba Town, North West Ethiopia. Int J Pharma Sci Res 2014; 5(10): 670–7.
- Suleman S, Ketsela A, Mekonnen Z. Assessment of self-medication practices in Assendabo town, Jimma zone, southwestern Ethiopia. Res Social Adm Pharm 2009; 5(1): 76–81.
- Mossa DA, Wabe NT, Angamo MT. Self-Medication with Antibiotics and Antimalarials in the Community of Silte Zone, South Ethiopia. TAF Prevent Med Bull 2012; 11(5): 529–36.
- Abay M, Amelo W. Assessment of Self-Medication Practices Among Medical, Pharmacy, and Health Science Students in Gondar University, Ethiopia. J Young Pharm 2010; 2(3): 306–10.
- Nagarajaiah B, Kishore M, Shashi K, Praveen P. Prevalence and pattern of self-medication practices among population of three districts of South Karnataka. Natl J Physiol Pharm Pharmacol 2016; 6(4): 296–300.
- Eticha T, Mesfin K. Self-Medication Practices in Mekelle, Ethiopia. PLoS ONE 2014; 9(5): e97464.
- Jasim AL, Fadhil TA, Taher SS. Self Medication Practice among Iraqi Patients in Baghdad City. Am J Pharmacol Sci 2014; 2(1): 18–23.
- El-Nimr NA, Wahdan IMH, Wahdan AMH, Kotb RE. Self-medication with drugs and complementary and alternative medicines in Alexandria, Egypt: prevalence, patterns and determinants. East Mediterr Health J 2015; 21(4): 256–65.
- Ararsa A, Bekele A. Assessment of Self-Medication Practice and Drug Storage on Private Pharmacy Clients in Jimma town, Oromia, South west Ethiopia. ARC J Pharm Sci 2015; 1(1): 20–32.
- Wen Y, Lieber E, Wan D, Hong Y. A qualitative study about self-medication in the community among market venders in Fuzhou, China. Health Soc Care Community 2011; 19(5): 504–13.
- Annadurai K, Selvasri S, Ramasamy J. Self-medication: predictors and practices among rural population of Nellikuppam Village, Kancheepuram District, Tamil Nadu. J Krishna Inst Med Sci 2017; 6(1): 90–98.
- Shankar PR, Partha P, Shenoy N. Self-medication and non-doctor prescription practices in Pokhara valley, Western Nepal: a questionnaire-based study. BMC Fam Pract 2002; 3: 17.
- Galato D, de Mattos Galafassi L, Modolon Alano G, Trauthman SC. Responsible self-medication: review of the process of pharmaceutical attendance. Braz J Pharm Sci 2009; 45(4): 625–33.
- Bennadi D. Self-medication: A current challenge. J Basic Clin Pharm 2014; 5(1): 19–23.
- Divya M, Bharatesh S, Vasudeva G, Varalakshmi C. Self-Medication Among Adults in Urban Udupi Taluk, Southern India. Int J Med Public Health 2016; 6(3): 126–9.
- Sado E, Gedif T. Drug utilization at household level in Nekemte town and surrounding rural areas, western Ethiopia: a cross-sectional study. Open Access Library J 2014; 1: e651.
- Mekonnen T. Self-medication practices with antibiotics among urban dwellers of Bahir Dar town. North West Ethiopia. Thesis, Adis Ababa Uuniversity Istitutional Repository 2014.
- Jafari F, Khatony A, and Rahmani E. Prevalence of Self-Medication Among the Elderly in Kermanshah-Iran. Glob J Health Sci 2015; 7(2): 360–65.
- Adzic Lukovic J, Miletić V, Pekmezovic T et al. Self-Medication Practices and Risk Factors for Self-Medication among Medical Students in Belgrade, Serbia. PLoS ONE 2014; 9(12): e114644.
- Bekele SA, Argaw MD, Yalew AW. Magnitude and Factors Associated with Self-Medication Practices among University Students: The Case of Arsi University, College of Health Science, Asella, Ethiopia: Cross-Sectional Survey Based Study. Open Access Library J 2016; 3: e2738.
- Abdulraheem IS, Adegboye A, Fatiregun AA. Self-medication with Antibiotics: Empirical Evidence from a Nigerian Rural Population. J Pharm Res Int 2016; 11(5): 1–13.
- Jain M, Prakash R, Bapna D, Jain R. Prevalence and Pattern of Selfmedication Practices in Urban area of Southern Rajasthan. Ntl J of Community Med 2015; 6(4): 474–77.
- Ahmad A, Khan MU, Srikanth AB, et al. Evaluation of KAP about Self-medication Among Rural and Urban North Indian Population. Int J Pharm Clin Res 2015; 7(5): 326–32.
- Angamo MT, Wabe NT. Knowledge, attitude and practice of self medication in southwest Ethiopia. Intl J Pharm Sci Res 2012; 3(4): 1005–10.